Abstract
Introduction
Recent data suggest patients with early-onset rectal cancer (EORC) receive neoadjuvant radiation above recommended doses without oncologic benefit. The use of excessive radiation may lead to worse outcomes and patient harm. We sought to evaluate predictors of aggressive neoadjuvant radiation (A-XRT) use in EORC patients and compare this to late-onset rectal cancer (LORC) patients.
Methods
The National Cancer Database from 2004 to 2014 was queried for rectal adenocarcinoma patients undergoing surgical resection. Patients with stage 0 or IV disease, positive margins, and incomplete data were excluded. Standard neoadjuvant radiation (S-XRT) was based upon NCCN guidelines: 25–50.4 Gray for stage II/III patients and none for stage I. Excess radiation was considered A-XRT. Patients diagnosed at age < 50 years were labeled EORC; those ≥ 50 years were LORC. Categorical data were analyzed with chi-square test. Logistic regression was used to analyze clinicodemographic associations with A-XRT.
Results
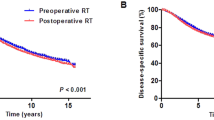
45,403 patients were included: 7999 (17.6%) EORC and 37,404 (82.4%) LORC. Multivariable logistic regression demonstrated that A-XRT use among stage I patient was associated with male gender, age under 50, urban location, mucinous histology, and poor tumor differentiation. Among stage II and III patients, A-XRT use was associated with male gender, age under 50, higher education and income, and urban location. Cox hazards did not demonstrate a significant association of A-XRT use with survival.
Conclusion
Our data reaffirm that EORC patients more frequently receive A-XRT and that use is based on demographic features independent of tumor characteristics. Reasons for A-XRT, particularly in EORC patients, should be clarified to promote adherence to guidelines and minimize patient harm.


Similar content being viewed by others
References
National Comprehensive Cancer Network (2020) Rectal cancer (version 1.2020). National Comprehensive Cancer Network, Bethesdas
Kolarich A, George TJ, Hughes SJ, Delitto D, Allegra CJ, Hall WA, Chang GJ, Tan SA, Shaw CM, Iqbal A (2018) Rectal cancer patients younger than 50 years lack a survival benefit from NCCN guideline–directed treatment for stage II and III disease. Cancer 124:3510–3519. https://doi.org/10.1002/cncr.31527
You YN, Dozois EJ, Boardman LA, Aakre J, Huebner M, Larson DW (2011) Young-onset rectal cancer: presentation, pattern of care and long-term oncologic outcomes compared to a matched older-onset cohort. Ann Surg Oncol 18:2469–2476. https://doi.org/10.1245/s10434-011-1674-7
Burbach JPM, Den Harder AM, Intven M, Van Vulpen M, Verkooijen HM, Reerink O (2014) Impact of radiotherapy boost on pathological complete response in patients with locally advanced rectal cancer: a systematic review and meta-analysis. Radiother Oncol. https://doi.org/10.1016/j.radonc.2014.08.035
Van Wickle JD, Paulson ES, Landry JC, Erickson BA, Hall WA (2017) Adaptive radiation dose escalation in rectal adenocarcinoma: a review. J. Gastrointest. Oncol. 8(5):902–914
Appelt AL, Ploen J, Vogelius IR, Bentzen SM, Jakobsen A (2013) Radiation dose-response model for locally advanced rectal cancer after preoperative chemoradiation therapy. Int J Radiat Oncol Biol Phys. https://doi.org/10.1016/j.ijrobp.2012.05.017
Chang DT, Pai RK, Rybicki LA, Dimaio MA, Limaye M, Jayachandran P, Koong AC, Kunz PA, Fisher GA, Ford JM, Welton M, Shelton A, Ma L, Arber DA, Pai RK (2012) Clinicopathologic and molecular features of sporadic early-onset colorectal adenocarcinoma: an adenocarcinoma with frequent signet ring cell differentiation, rectal and sigmoid involvement, and adverse morphologic features. Mod Pathol 25:1128–1139. https://doi.org/10.1038/modpathol.2012.61
Mistry SA, Madala H, Chacko C, Gernand J, Logrono A, Arora ML, Kakarala R (2014) Rectal cancer: Characteristics and survival rates of young versus old. J Clin Oncol 32:14517. https://doi.org/10.1200/jco.2014.32.15_suppl.e14517
Ofshteyn A, Bingmer K, Dorth J, Dietz D, Steinhagen E, Stein SL (2020) Disparities in neoadjuvant radiation dosing for treatment of rectal cancer. Am J Surg 220:987–992. https://doi.org/10.1016/j.amjsurg.2020.01.016
Nicholas S, Chen L, Choflet A, Fader A, Guss Z, Hazell S, Song DY, Tran PT, Viswanathan AN (2017) Pelvic radiation and normal tissue toxicity. Semin Radiat Oncol 27(4):358–369
Nakamura K, Konishi K, Komatsu T, Ishiba R (2019) Quality of life after external beam radiotherapy for localized prostate cancer: comparison with other modalities. Int J Urol 26:950–954. https://doi.org/10.1111/iju.14026
Rombouts AJM, Hugen N, Elferink MAG, Feuth T, Poortmans PMP, Nagtegaal ID, de Wilt JHW (2017) Incidence of second tumors after treatment with or without radiation for rectal cancer. Ann Oncol. https://doi.org/10.1093/annonc/mdw661
Lorimer PD, Motz BM, Kirks RC, Boselli DM, Walsh KK, Prabhu RS, Hill JS, Salo JC (2017) Pathologic complete response rates after neoadjuvant treatment in rectal cancer: an analysis of the national cancer database. Ann Surg Oncol. https://doi.org/10.1245/s10434-017-5873-8
Burnett-Hartman AN, Powers JD, Chubak J, Corley DA, Ghai NR, McMullen CK, Pawloski PA, Sterrett AT, Feigelson HS (2019) Treatment patterns and survival differ between early-onset and late-onset colorectal cancer patients: the patient outcomes to advance learning network. Cancer Causes Control. https://doi.org/10.1007/s10552-019-01181-3
Weinberg BA, Marshall JL, Salem ME (2017) The growing challenge of young adults with colorectal cancer. Oncology (Williston Park) 31(5):381–389
Wiltshire KL, Ward IG, Swallow C, Oza AM, Cummings B, Pond GR, Catton P, Kim J, Ringash J, Wong CS, Wong R, Siu LL, Moore M, Brierley J (2006) Preoperative radiation with concurrent chemotherapy for resectable rectal cancer: effect of dose escalation on pathologic complete response, local recurrence-free survival, disease-free survival, and overall survival. Int J Radiat Oncol Biol Phys. https://doi.org/10.1016/j.ijrobp.2005.08.012
Funding
The authors received no financial support for the research and authorship of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Stein has served as a guest speaker for the Merck Sharp & Dohme Corporation. Drs. Bliggenstorfer, Bingmer, Ofshteyn, Charles, and Steinhagen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bliggenstorfer, J.T., Bingmer, K., Ofshteyn, A. et al. Neoadjuvant radiation above NCCN guidelines for rectal cancer is associated with age under 50 and early clinical stage. Surg Endosc 36, 2925–2935 (2022). https://doi.org/10.1007/s00464-021-08585-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08585-w