Abstract
Background
The lesion detection rate of esophagogastroduodenoscopy (EGD) varies depending on the degree of experience of the endoscopist and anatomical blind spots. This study aimed to identify gaze patterns and blind spots by analyzing the endoscopist’s gaze during real-time EGD.
Methods
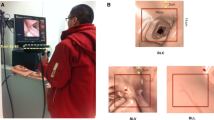
Five endoscopists were enrolled in this study. The endoscopist’s eye gaze tracked by an eye tracker was selected from the esophagogastric junction to the second portion of the duodenum without the esophagus during insertion and withdrawal, and then matched with photos. Gaze patterns were visualized as a gaze plot, blind spot detection as a heatmap, observation time (OT), fixation duration (FD), and FD-to-OT ratio.
Results
The mean OT and FD were 11.10 ± 11.14 min and 8.37 ± 9.95 min, respectively, and the FD-to-OT ratio was 72.5%. A total of 34.3% of the time was spent observing the antrum. When observing the body of the stomach, it took longer to observe the high body in the retroflexion view and the low-to-mid body in the forward view.
Conclusions
It is necessary to minimize gaze distraction and observe the posterior wall in the retroflexion view. Our results suggest that eye-tracking techniques may be useful for future endoscopic training and education.



Similar content being viewed by others
References
Min JK et al (2018) Revision of quality indicators for the endoscopy quality improvement program of the national cancer screening program in Korea. The Korean Journal of Gastroenterology = Taehan Sohwagi Hakhoe Chi 71:269–281. https://doi.org/10.4166/kjg.2018.71.5.269
Chadwick G et al (2015) Gastric cancers missed during endoscopy in England. Clin Gastroenterol Hepatol 13:1264-1270.e1. https://doi.org/10.1016/j.cgh.2015.01.025
Chadwick G et al (2014) A population-based, retrospective, cohort study of esophageal cancer missed at endoscopy. Endoscopy 46:553–560. https://doi.org/10.1055/s-0034-1365646
Wang YR, Loftus EV, Judge TA, Peikin SR (2016) Rate and predictors of interval esophageal and gastric cancers after esophagogastroduodenoscopy in the United States. Digestion 94:176–180. https://doi.org/10.1159/000452794
Pimenta-Melo AR, Monteiro-Soares M, Libânio D, Dinis-Ribeiro M (2016) Missing rate for gastric cancer during upper gastrointestinal endoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 28:1041–1049. https://doi.org/10.1097/MEG.0000000000000657
Visrodia K et al (2016) Magnitude of missed esophageal adenocarcinoma after Barrett’s esophagus diagnosis: a systematic review and meta-analysis. Gastroenterology 150:599-607.e597. https://doi.org/10.1053/j.gastro.2015.11.040 (quiz e514-595)
Moon HS (2015) Improving the endoscopic detection rate in patients with early gastric cancer. Clin Endosc 48:291–296. https://doi.org/10.5946/ce.2015.48.4.291
Chiu PWY (2018) Editorial on quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Transl Gastroenterol Hepatol 3:13–13. https://doi.org/10.21037/tgh.2018.01.05
Rex DK et al (2015) Quality indicators for colonoscopy. Gastrointest Endosc 81:31–53. https://doi.org/10.1016/j.gie.2014.07.058
Oh JR et al (2018) Colonoscopy learning curves for colorectal surgery fellow trainees: experiences with the 15-year colonoscopy training program. Ann Surg Treat Res 95:169–174. https://doi.org/10.4174/astr.2018.95.4.169
He W et al (2020) Eye gaze of endoscopists during simulated colonoscopy. J Robot Surg 14:137–143. https://doi.org/10.1007/s11701-019-00950-1
Kim JS, Kim BW (2017) Training in endoscopy: esophagogastroduodenoscopy. Clin Endosc 50:318–321. https://doi.org/10.5946/ce.2017.096
Bisschops R et al (2016) Performance measures for upper gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy 48:843–864. https://doi.org/10.1055/s-0042-113128
Park WG et al (2015) Quality indicators for EGD. Gastrointest Endosc 81:17–30. https://doi.org/10.1016/j.gie.2014.07.057
Teh JL et al (2015) Longer examination time improves detection of gastric cancer during diagnostic upper gastrointestinal endoscopy. Clin Gastroenterol Hepatol 13:480-487.e2. https://doi.org/10.1016/j.cgh.2014.07.059
Park JM et al (2017) Longer observation time increases proportion of neoplasms detected by esophagogastroduodenoscopy. Gastroenterology 153:460-469.e1. https://doi.org/10.1053/j.gastro.2017.05.009
Marques S, Bispo M, Pimentel-Nunes P, Chagas C, Dinis-Ribeiro M (2017) Image documentation in gastrointestinal endoscopy: review of recommendations. GE Port J Gastroenterol 24:269–274. https://doi.org/10.1159/000477739
Beg S et al (2017) Quality standards in upper gastrointestinal endoscopy: a position statement of the British Society of Gastroenterology (BSG) and Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland (AUGIS). Gut 66:1886–1899. https://doi.org/10.1136/gutjnl-2017-314109
McCarley JS, Kramer AF, Wickens CD, Vidoni ED, Boot WR (2004) Visual skills in airport-security screening. Psychol Sci 15:302–306. https://doi.org/10.1111/j.0956-7976.2004.00673.x
Khan MQ, Lee S (2019) Gaze and eye tracking: techniques and applications in ADAS. Sensors 19:5540. https://doi.org/10.3390/s19245540
Al-Moteri MO, Symmons M, Plummer V, Cooper S (2017) Eye tracking to investigate cue processing in medical decision-making: a scoping review. Comput Hum Behav 66:52–66. https://doi.org/10.1016/j.chb.2016.09.022
Blondon K, Wipfli R, Lovis C (2015) Use of eye-tracking technology in clinical reasoning: a systematic review. Stud Health Technol Inform 210:90–94
den Boer L et al (2018) Volumetric image interpretation in radiology: scroll behavior and cognitive processes. Adv Health Sci Educ 23:783–802. https://doi.org/10.1007/s10459-018-9828-z
Lami M et al (2018) Gaze patterns hold key to unlocking successful search strategies and increasing polyp detection rate in colonoscopy. Endoscopy 50:701–707. https://doi.org/10.1055/s-0044-101026
Dik VK, Hooge IT, van Oijen MG, Siersema PD (2016) Measuring gaze patterns during colonoscopy: a useful tool to evaluate colon inspection? Eur J Gastroenterol Hepatol 28:1400–1406. https://doi.org/10.1097/MEG.0000000000000717
Almansa C, Shahid MW, Heckman MG, Preissler S, Wallace MB (2011) Association between visual gaze patterns and adenoma detection rate during colonoscopy: a preliminary investigation. Am J Gastroenterol 106:1070–1074. https://doi.org/10.1038/ajg.2011.26
Kumahara K et al (2019) Objective evaluation of the visibility of colorectal lesions using eye tracking. Dig Endosc 31:552–557. https://doi.org/10.1111/den.13397
Meining A, Atasoy S, Chung A, Navab N, Yang GZ (2010) ‘Eye-tracking’ for assessment of image perception in gastrointestinal endoscopy with narrow-band imaging compared with white-light endoscopy. Endoscopy 42:652–655. https://doi.org/10.1055/s-0029-1244233
Whitehead AL, Julious SA, Cooper CL, Campbell MJ (2016) Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res 25:1057–1073. https://doi.org/10.1177/0962280215588241
Yao K (2013) The endoscopic diagnosis of early gastric cancer. Ann Gastroenterol 26:11–22
Brunyé TT, Drew T, Weaver DL, Elmore JG (2019) A review of eye tracking for understanding and improving diagnostic interpretation. Cogn Res 4:7. https://doi.org/10.1186/s41235-019-0159-2
Liversedge SP, Findlay JM (2000) Saccadic eye movements and cognition. Trends Cogn Sci 4:6–14
Findlay JM, Findlay JM, Gilchrist ID (2003) Active vision: the psychology of looking and seeing. Oxford University Press, Oxford
Rayner K (1998) Eye movements in reading and information processing: 20 years of research. Psychol Bull 124:372–422
Liversedge S, Gilchrist I, Everling S (2011) The Oxford handbook of eye movements. Oxford University Press, Oxford
Holmqvist K et al (2011) Eye tracking: a comprehensive guide to methods and measures. OUP Oxford, Oxford
Stewart EEM, Valsecchi M, Schütz AC (2020) A review of interactions between peripheral and foveal vision. J Vis 20:2–2. https://doi.org/10.1167/jov.20.12.2 (%JJournalofVision (2020))
Larson AM, Loschky LC (2009) The contributions of central versus peripheral vision to scene gist recognition. J Vis 9:6. https://doi.org/10.1167/9.10.6
Arnold SH, Svendsen MB, Konge L, Svendsen LB, Preisler L (2015) Three-dimensional motion tracking correlates with skill level in upper gastrointestinal endoscopy. Endoscopy 47:825–828. https://doi.org/10.1055/s-0034-1391884
Acknowledgements
The authors would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
Each author’s individual contributions are as below: AL, YC, and HC analyzed and drafted the manuscript; AL and HC designed the study and edited the manuscript; HC, SC, and SGK provided critical revision of the manuscript for important intellectual content; YC, EL, and JLK provided statistical support; YC, HC, JC, BK, and SC provided data acquisition; HC and SGK supervised the study. All the authors approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
The authors Ayoung Lee, Hyunsoo Chung, Yejin Cho, Jue Lie Kim, Jinju Choi, Eunwoo Lee, Bokyung Kim, Soo-Jeong Cho, and Sang Gyun Kim have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, A., Chung, H., Cho, Y. et al. Identification of gaze pattern and blind spots by upper gastrointestinal endoscopy using an eye-tracking technique. Surg Endosc 36, 2574–2581 (2022). https://doi.org/10.1007/s00464-021-08546-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08546-3