Abstract
Background
Self-expanding metallic stents (SEMSs) are used as a bridge to surgery in patients with obstructive colorectal cancer. However, the role of laparoscopic resection after successful stent deployment is not well established. We aimed to compare the oncologic outcomes of laparoscopic vs open surgery after successful colonic stent deployment in patients with obstructive left-sided colorectal cancer.
Methods
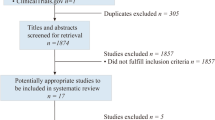
In this multicenter study, 179 (97 laparoscopy, 82 open surgery) patients with obstructive left-sided colorectal cancer who underwent radical resection with curative intent after successful stent deployment were retrospectively reviewed. To minimize bias, we used inverse probability treatment-weighted propensity score analysis. The short- and long-term outcomes between the groups were compared.
Results
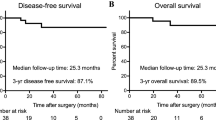
Both groups had similar demographic and tumor characteristics. The operation time was longer, but the degree of blood loss was lower in the laparoscopy than in the open surgery group. There were nine (9.3%) open conversions. After adjustment, the groups showed similar patient and tumor characteristics. The 5-year disease-free survival (DFS) (laparoscopic vs open: 68.7% vs 48.5%, p = 0.230) and overall survival (OS) (laparoscopic vs open: 79.1% vs 69.0%, p = 0.200) estimates did not differ significantly across a median follow-up duration of 50.5 months. Advanced stage disease (DFS: hazard ratio [HR] 1.825, 95% confidence interval [CI]: 1.072–3.107; OS: HR 2.441, 95% CI 1.216–4.903) and post-operative chemotherapy omission (DFS: HR 2.529, 95% CI 1.481–4.319; OS: HR 2.666, 95% CI 1.370–5.191) were associated with relatively worse long-term outcomes.
Conclusion
Stent insertion followed by laparoscopy with curative intent is safe and feasible; the addition of post-operative chemotherapy should be considered after successful treatment.



Similar content being viewed by others
References
Mangano A, Motson RW (2016) Evidence-based analysis of self-expanding metallic stent as a bridge to surgery versus emergency surgery for colon cancer. Future Oncol 12:1957–1960
Tan CJ, Dasari BVM, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99:469–476
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Lutke Holzik MF, Grubben MJ, Sprangers MA, Dijkgraaf MG, Fockens P, Collaborative Dutch Stent-In Study G (2011) Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol 12:344–352
Amelung FJ, Borstlap WAA, Consten ECJ, Veld JV, van Halsema EE, Bemelman WA, Siersema PD, Ter Borg F, van Hooft JE, Tanis PJ, Dutch Snapshot Research G (2019) Propensity score-matched analysis of oncological outcome between stent as bridge to surgery and emergency resection in patients with malignant left-sided colonic obstruction. Br J Surg 106:1075–1086
Kang SI, Oh H-K, Yoo JS, Ahn S, Kim MH, Kim MJ, Son IT, Kim D-W, Kang S-B, Park YS, Yoon CJ, Shin R, Heo SC, Lee IT, Youk EG, Kim MJ, Chang TY, Park S-C, Sohn DK, Oh JH, Park JW, Ryoo S-B, Jeong S-Y, Park KJ (2018) Oncologic outcomes of preoperative stent insertion first versus immediate surgery for obstructing left-sided colorectal cancer. Surg Oncol 27:216–224
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM, Group COcLoORS (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477-484
Kang SB, Park JW, Jeong SY, Nam BH, Choi HS, Kim DW, Lim SB, Lee TG, Kim DY, Kim JS, Chang HJ, Lee HS, Kim SY, Jung KH, Hong YS, Kim JH, Sohn DK, Kim DH, Oh JH (2010) Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 11:637–645
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Colon Cancer Laparoscopic or Open Resection Study G, Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Newman CM, Arnold SJ, Coull DB, Linn TY, Moran BJ, Gudgeon AM, Cecil TD (2012) The majority of colorectal resections require an open approach, even in units with a special interest in laparoscopic surgery. Colorectal Dis 14:29–34
Allaix ME, Furnee EJ, Mistrangelo M, Arezzo A, Morino M (2016) Conversion of laparoscopic colorectal resection for cancer: What is the impact on short-term outcomes and survival? World J Gastroenterol 22:8304–8313
Scheidbach H, Garlipp B, Oberlander H, Adolf D, Kockerling F, Lippert H (2011) Conversion in laparoscopic colorectal cancer surgery: impact on short- and long-term outcome. J Laparoendosc Adv Surg Tech A 21:923–927
Punt CJ, Buyse M, Kohne CH, Hohenberger P, Labianca R, Schmoll HJ, Pahlman L, Sobrero A, Douillard JY (2007) Endpoints in adjuvant treatment trials: a systematic review of the literature in colon cancer and proposed definitions for future trials. J Natl Cancer Inst 99:998–1003
Heinze G, Juni P (2011) An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J 32:1704–1708
Cole SR, Hernan MA (2004) Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed 75:45–49
National Comprehensive Cancer Network (2019) NCCN Guidelines Colon Cancer (version 2. 2019). http://www.nccn.org/. Accessed 5 Aug 2019
van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Gotz M, van Halsema EE, Hill J, Manes G, Meisner S, Rodrigues-Pinto E, Sabbagh C, Vandervoort J, Tanis PJ, Vanbiervliet G, Arezzo A (2020) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2020. Endoscopy 52:389–407
Chung TS, Lim SB, Sohn DK, Hong CW, Han KS, Choi HS, Jeong SY (2008) Feasibility of single-stage laparoscopic resection after placement of a self-expandable metallic stent for obstructive left colorectal cancer. World J Surg 32:2275–2280
Shimizu H, Yamazaki R, Ohtsuka H, Osaka I, Takuma K, Morita Y (2018) Feasibility of laparoscopic surgery after stent insertion for obstructive colorectal cancer. Asian Journal of Endoscopic Surgery 11:118–122
Enomoto T, Saida Y, Takabayashi K, Nagao S, Takeshita E, Watanabe R, Takahashi A, Nakamura Y, Asai K, Watanebe M, Nagao J, Kusachi S (2016) Open surgery versus laparoscopic surgery after stent insertion for obstructive colorectal cancer. Surg Today 46:1383–1386
Rho SY, Bae SU, Baek SJ, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2013) Feasibility and safety of laparoscopic resection following stent insertion for obstructing left-sided colon cancer. Journal of the Korean Surgical Society 85:290–295
Bae SU, Yang CS, Kim S, Lim DR, Jeong WK, Dong Kim D, Kim JH, Shin EJ, Lee YJ, Lee JY, Kim NK, Baek SK (2019) Long-term oncologic outcomes of laparoscopic versus open resection following stent insertion for obstructing colon cancer: a multi-center retrospective study. Surg Endosc 33:3937–3944
Meyers BM, Cosby R, Quereshy F, Jonker D (2017) Adjuvant Chemotherapy for Stage II and III Colon Cancer Following Complete Resection: A Cancer Care Ontario Systematic Review. Clin Oncol (R Coll Radiol) 29:459–465
Labianca R, Nordlinger B, Beretta GD, Mosconi S, Mandala M, Cervantes A, Arnold D, Group EGW (2013) Early colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 24 Suppl 6: vi64–72
Figueredo A, Coombes ME, Mukherjee S (2008) Adjuvant therapy for completely resected stage II colon cancer. Cochrane Database Syst Rev 16:CD005390.
Kim HJ, Choi GS, Park JS, Park SY, Jun SH (2013) Higher rate of perineural invasion in stent-laparoscopic approach in comparison to emergent open resection for obstructing left-sided colon cancer. Int J Colorectal Dis 28:407–414
Yamashita S, Tanemura M, Sawada G, Moon J, Shimizu Y, Yamaguchi T, Kuwai T, Urata Y, Kuraoka K, Hatanaka N, Yamashita Y, Taniyama K (2018) Impact of endoscopic stent insertion on detection of viable circulating tumor cells from obstructive colorectal cancer. Oncol Lett 15:400–406
Maruthachalam K, Lash GE, Shenton BK, Horgan AF (2007) Tumor cell dissemination following endoscopic stent insertion. Br J Surg 94:1151–1154
Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Kawano Y, Yamahatsu K, Sekiguchi K, Yamada M, Hatori T, Yoshida H (2018) Colonic stent-induced mechanical compression may suppress cancer cell proliferation in malignant large bowel obstruction. Surg Endosc 33:1290–1297
Acknowledgements
An abstract version of this article was presented at the 13th Scientific and Annual Meeting of European Society of Coloproctology 2018. None of the authors have commercial associations (e.g., consultancies, stock ownership, equity interests, patent-licensing arrangements, research support, speaking fees) that may pose a conflict of interest in connection with this study. We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
This work was supported by a Grant (No. 02-2018-036) from the SNUBH Research Fund.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Drs. Min Hyun Kim, Sung Il Kang, Jeehye Lee, Heung-Kwon Oh, Soyeon Ahn, Duck-Woo Kim, Sung-Bum Kang, Rumi Shin, Seung Chul Heo, Eui Gon Youk, Sung-Chan Park, Dae Kyung Sohn, Jae Hwan Oh, Min Jung Kim, Ji Won Park, Seung-Bum Ryoo, Seung-Yong Jeong, and Kyu Joo Park have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, M.H., Kang, S.I., Lee, J. et al. Oncologic safety of laparoscopic surgery after metallic stent insertion for obstructive left-sided colorectal cancer: a multicenter comparative study. Surg Endosc 36, 385–395 (2022). https://doi.org/10.1007/s00464-021-08293-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08293-5