Abstract
Background
Despite literature and guidelines recommending same admission cholecystectomy (CCY) after endoscopic retrograde cholangiopancreatography (ERCP) for patients with acute gallstone pancreatitis, clinical practice remains variable. The aim of this study was to investigate the role of clinical and socio-demographic factors in the management of acute gallstone pancreatitis.
Methods
Patients with acute gallstone pancreatitis who underwent ERCP during hospitalization were reviewed from the U.S. Nationwide Inpatient Sample database between 2008 and 2014. Patients were classified by treatment strategy: ERCP + same admission CCY (ERCP + CCY) versus ERCP alone. Measured variables including age, race/ethnicity, Charlson Comorbidity Index (CCI), hospital type/region, insurance payer, household income, length of hospital stay (LOS), hospitalization cost, and in-hospital mortality were compared between cohorts using χ2 and ANOVA. Multivariable logistic regression was performed to identify specific predictors of same admission CCY.
Results
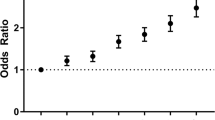
A total of 205,012 patients (ERCP + CCY: n = 118,318 versus ERCP alone: n = 86,694) were analyzed. A majority (53.4%) of patients that did not receive same admission CCY were at urban-teaching hospitals. LOS was longer with higher associated costs for patients with same admission CCY [(6.8 ± 5.6 versus 6.4 ± 6.5 days; P < 0.001) and ($69,135 ± 65,913 versus $52,739 ± 66,681; P < 0.001)]. Mortality was decreased significantly for patients who underwent ERCP + CCY versus ERCP alone (0.4% vs 1.1%; P < 0.001). Multivariable regression demonstrated female gender, Black race, higher CCI, Medicare payer status, urban-teaching hospital location, and household income decreased the odds of undergoing same admission CCY + ERCP (all P < 0.001).
Conclusion
Based upon this analysis, multiple socioeconomic and healthcare-related disparities influenced the surgical management of acute gallstone pancreatitis. Further studies to investigate these disparities are indicated.

Similar content being viewed by others
References
Peery AF, Crockett SD, Barritt AS et al (2015) Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology 149(7):1731-1741.e1733
Peery AF, Crockett SD, Murphy CC et al (2019) Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology 156(1):254-272.e211
Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN, American Gastroenterological Association Institute Clinical Guidelines Committee (2018) American Gastroenterological Association Institute guideline on initial management of acute pancreatitis. Gastroenterology 154(4):1096–1101
Forsmark CE, Baillie J, AGA Institute Clinical Practice and Economics Committee, AGA Institute Governing Board (2007) AGA Institute technical review on acute pancreatitis. Gastroenterology 132(5):2022–2044
Gullo L, Migliori M, Olah A et al (2002) Acute pancreatitis in five European countries: etiology and mortality. Pancreas 24(3):223–227
Forsmark CE, Vege SS, Wilcox CM (2016) Acute pancreatitis. N Engl J Med 375(20):1972–1981
Najafian N, McCarty TR (2018) Empagliflozin-associated pancreatitis: a case report and clinical review of drug-induced pancreatitis. Conn Med 82(9):543–546
Lerch MM, Saluja AK, Runzi M, Dawra R, Saluja M, Steer ML (1993) Pancreatic duct obstruction triggers acute necrotizing pancreatitis in the opossum. Gastroenterology 104(3):853–861
Opie EL, Meakins JC (1909) Data concerning the etiology and pathology of hemorrhagic necrosis of the pancreas (acute hemorrhagic pancreatitis). J Exp Med 11(4):561–578
Opie EL (1901) The etiology of acute hemorrhagic pancreatitis. Bull Johns Hopkins Hosp 12:182
Neoptolemos JP (1989) The theory of ‘persisting’ common bile duct stones in severe gallstone pancreatitis. Ann R Coll Surg Engl 71(5):326–331
ASoP Committee, Buxbaum JL, Abbas Fehmi SM et al (2019) ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc 89(6):1075–1105.e1015.
Uhl W, Muller CA, Krahenbuhl L, Schmid SW, Scholzel S, Buchler MW (1999) Acute gallstone pancreatitis: timing of laparoscopic cholecystectomy in mild and severe disease. Surg Endosc 13(11):1070–1076
Uhl W, Warshaw A, Imrie C et al (2002) IAP guidelines for the surgical management of acute pancreatitis. Pancreatology 2(6):565–573
Heij HA, Veen HF, Eggink WF, Obertop H (1985) Timing of surgery for acute biliary pancreatitis. Am J Surg 149(3):371–374
Ranson JH (1979) The timing of biliary surgery in acute pancreatitis. Ann Surg 189(5):654–663
Tondelli P, Stutz K, Harder F, Schuppisser JP, Allgower M (1982) Acute gallstone pancreatitis: best timing for biliary surgery. Br J Surg 69(12):709–710
da Costa DW, Bouwense SA, Schepers NJ et al (2015) Same admission versus interval cholecystectomy for mild gallstone pancreatitis (PONCHO): a multicentre randomised controlled trial. Lancet 386(10000):1261–1268
da Costa DW, Dijksman LM, Bouwense SA et al (2016) Cost-effectiveness of same admission versus interval cholecystectomy after mild gallstone pancreatitis in the PONCHO trial. Br J Surg 103(12):1695–1703
Leppaniemi A, Tolonen M, Tarasconi A et al (2019) 2019 WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg 14:27
Tenner S, Baillie J, DeWitt J, Vege SS, American College of Gastroenterology (2013) American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol 108(9):1400–1415; 1416
IAP/APA Acute Pancreatitis Guidelines Working Group (2013) IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 13(4 Suppl 2):e1–e15
Rebours V, Levy P, Bretagne JF, Bommelaer G, Hammel P, Ruszniewski P (2012) Do guidelines influence medical practice? Changes in management of acute pancreatitis 7 years after the publication of the French guidelines. Eur J Gastroenterol Hepatol 24(2):143–148
Nguyen GC, Tuskey A, Jagannath SB (2008) Racial disparities in cholecystectomy rates during hospitalizations for acute gallstone pancreatitis: a national survey. Am J Gastroenterol 103(9):2301–2307
Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP): advancing excellence in health care. https://www.ahrq.gov/research/data/hcup/index.html. Accessed 11 Nov 2019
McCarty TR, Echouffo-Tcheugui JB, Lange A, Haque L, Njei B (2018) Impact of bariatric surgery on outcomes of patients with nonalcoholic fatty liver disease: a nationwide inpatient sample analysis, 2004–2012. Surg Obes Relat Dis 14(1):74–80
Bilal M, Kline KT, Trieu JA et al (2019) Trends in same admission cholecystectomy and endoscopic retrograde cholangiopancreatography for acute gallstone pancreatitis: a nationwide analysis across a decade. Pancreatology 19(4):524–530
Healthcare Cost and Utilization Project (HCUP). Overview of National (Nationwide) Inpatient Sample (NIS). Accessed 15 Dec 2019
Tse F, Yuan Y (2012) Early routine endoscopic retrograde cholangiopancreatography strategy versus early conservative management strategy in acute gallstone pancreatitis. Cochrane Database Syst Rev (5):CD009779
Banks PA, Bollen TL, Dervenis C et al (2013) Classification of acute pancreatitis—2012: revision of the Atlanta Classification and definitions by international consensus. Gut 62(1):102–111
Kadiyala V, Suleiman SL, McNabb-Baltar J, Wu BU, Banks PA, Singh VK (2016) The Atlanta Classification, Revised Atlanta Classification, and determinant-based classification of acute pancreatitis: which is best at stratifying outcomes? Pancreas 45(4):510–515
Campbell EJ, Montgomery DA, MacKay CJ (2007) A survey of current surgical treatment of acute gallstone disease in the west of Scotland. Scott Med J 52(4):15–19
Campbell EJ, Montgomery DA, Mackay CJ (2008) A national survey of current surgical treatment of acute gallstone disease. Surg Laparosc Endosc Percutan Tech 18(3):242–247
Ong SK, Christie PM, Windsor JA (2003) Management of gallstone pancreatitis in Auckland: progress and compliance. ANZ J Surg 73(4):194–199
Gollust SE, Cunningham BA, Bokhour BG et al (2018) What causes racial health care disparities? A mixed-methods study reveals variability in how health care providers perceive causal attributions. Inquiry 55:46958018762840
Loehrer AP, Song Z, Auchincloss HG, Hutter MM (2015) Influence of health insurance expansion on disparities in the treatment of acute cholecystitis. Ann Surg 262(1):139–145
Funding
This work was funded, at least in part, by the NIH Grant T32 DK007533-35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Christopher C Thompson has the following disclosures: Apollo Endosurgery: Consultant/Research Support (Consulting fees/Institutional Research Grants), Aspire Bariatrics: Research Support (Institutional Research Grant), BlueFlame Healthcare Venture Fund: General Partner, Boston Scientific: Consultant (Consulting fees), Covidien/Medtronic: Consultant (Consulting Fees), EnVision Endoscopy (Board Member), Fractyl: Consultant/Advisory Board Member (Consulting Fees), GI Dynamics: Consultant (Consulting Fees)/Research Support (Institutional Research Grant), GI Windows: Ownership interest, Olympus/Spiration: Consultant (Consulting Fees)/Research Support (Equipment Loans), Spatz: Research Support (Institutional Research Grant), USGI Medical: Consultant (Consulting Fees)/Advisory Board Member (Consulting fees)/Research Support (Research Grant). Thiruvengadam Muniraj has the following disclosures: Boston Scientific: Consultant. Fouad Chouairi, Thomas R. McCarty, Kelly Hathorn, Prabin Sharma, Harry R. Aslanian, and Priya Jamidar have no conflicts of interest or financial ties to disclose.
Ethical approval
All authors approve of final submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chouairi, F., McCarty, T.R., Hathorn, K.E. et al. Evaluation of socioeconomic and healthcare disparities on same admission cholecystectomy after endoscopic retrograde cholangiopancreatography among patients with acute gallstone pancreatitis. Surg Endosc 36, 274–281 (2022). https://doi.org/10.1007/s00464-020-08272-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08272-2