Abstract
Background
The aim of this study was to identify national utilization trends of robotic surgery for elective colectomy, conversion rates over time, and the specific impact of conversion on postoperative morbidity. Conversion to open represents a hard endpoint for minimally invasive surgery (MIS) and is associated with worse outcomes when compared to MIS or even traditional open procedures.
Methods
All adult patients who underwent either laparoscopic or robotic elective colectomy from 2013 to 2018 as reported in the American College of Surgeons Quality Improvement Program (ACS-NSQIP) database were included. National trends of both robotic utilization and conversion rates were analyzed, overall and according to underlying disease (benign disease, inflammatory bowel disease (IBD), cancer), or the presence of obesity (body mass index (BMI) ≥ 30 kg/m2). Demographic and surgical risk factors for surgical conversion to open were identified through multivariable regression analysis. Further assessed were overall and specific postoperative 30-day complications, which were risk adjusted and compared between converted patients and the remaining cohort.
Results
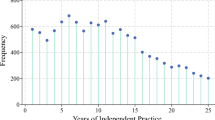
Of 66,652 included procedures, 5353 (8.0%) were converted to open. Conversion rates were 8.5% for laparoscopic and 4.9% for robotic surgery (p < 0.0001). A decline in conversion rates over the 6-year inclusion period was observed overall and for patients with obesity. This trend paralleled an increased utilization of the robotic platform. Several surrogates for advanced disease stages for cancer, diverticulitis, and IBD and prolonged surgical duration were identified as independent risk factors for unplanned conversion, while robotic approach was an independent protective factor (OR 0.44, p < 0.0001). Patients who had unplanned conversion were more likely to experience postoperative complications (OR 2.36; 95% CI [2.21–2.51]), length of hospital stay ≥ 6 days (OR 2.86; 95% CI [2.67–3.05], and 30-day mortality (OR 2.28; 95% CI [1.72–3.02]).
Conclusion
This nationwide study identified a decreasing trend in conversion rates over the 6-year inclusion period, both overall and in patients with obesity, paralleling increased utilization of the robotic platform. Unplanned conversion to open was associated with a higher risk of postoperative complications.


Similar content being viewed by others
References
Zhao JH, Sun JX, Huang XZ, Gao P, Chen XW, Song YX et al (2016) Meta-analysis of the laparoscopic versus open colorectal surgery within fast track surgery. Int J Colorectal Dis 31(3):613–622
Goh BK (2007) Impact of laparoscopic resection for colorectal cancer on operative outcomes and survival. Ann Surg 246(2):338–339
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372(14):1324–1332
Simillis C, Lal N, Thoukididou SN, Kontovounisios C, Smith JJ, Hompes R et al (2019) Open versus laparoscopic versus robotic versus transanal mesorectal excision for rectal cancer: a systematic review and network meta-analysis. Ann Surg 270(1):59–68
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J et al (2019) Robotic-assisted surgery compared with laparoscopic resection surgery for rectal cancer: the ROLARR RCT. Effic Mech Eval. https://doi.org/10.3310/eme06100
Corrigan N, Marshall H, Croft J, Copeland J, Jayne D, Brown J (2018) Exploring and adjusting for potential learning effects in ROLARR: a randomised controlled trial comparing robotic-assisted vs. standard laparoscopic surgery for rectal cancer resection. Trials 19(1):339
Crippa J, Grass F, Achilli P, Mathis KL, Kelley SR, Merchea A et al (2020) Risk factors for conversion in laparoscopic and robotic rectal cancer surgery. Br J Surg 107(5):560–566
Crippa J, Grass F, Dozois EJ, Mathis KL, Merchea A, Colibaseanu DT et al (2020) Robotic surgery for rectal cancer provides advantageous outcomes over laparoscopic approach: results from a large retrospective cohort. Ann Surg. https://doi.org/10.1097/sla.0000000000003805
Panteleimonitis S, Pickering O, Abbas H, Harper M, Kandala N, Figueiredo N et al (2018) Robotic rectal cancer surgery in obese patients may lead to better short-term outcomes when compared to laparoscopy: a comparative propensity scored match study. Int J Colorectal Dis 33(8):1079–1086
Duchalais E, Machairas N, Kelley SR, Landmann RG, Merchea A, Colibaseanu DT et al (2018) Does obesity impact postoperative outcomes following robotic-assisted surgery for rectal cancer? Surg Endosc 32(12):4886–4892
Lee YF, Albright J, Akram WM, Wu J, Ferraro J, Cleary RK (2018) Unplanned robotic-assisted conversion-to-open colorectal surgery is associated with adverse outcomes. J Gastrointest Surg 22(6):1059–1067
Bastawrous AL, Landmann RG, Liu Y, Liu E, Cleary RK (2020) Incidence, associated risk factors, and impact of conversion to laparotomy in elective minimally invasive sigmoidectomy for diverticular disease. Surg Endosc 34(2):598–609
Al-Temimi MH, Chandrasekaran B, Agapian J, Peters WR Jr, Wells KO (2019) Robotic versus laparoscopic elective colectomy for left side diverticulitis: a propensity score-matched analysis of the NSQIP database. Int J Colorectal Dis 34(8):1385–1392
Dolejs SC, Waters JA, Ceppa EP, Zarzaur BL (2017) Laparoscopic versus robotic colectomy: a national surgical quality improvement project analysis. Surg Endosc 31(6):2387–2396
Spinoglio G, Bianchi PP, Marano A, Priora F, Lenti LM, Ravazzoni F et al (2018) Robotic versus laparoscopic right colectomy with complete mesocolic excision for the treatment of colon cancer: perioperative outcomes and 5-year survival in a consecutive series of 202 patients. Ann Surg Oncol 25(12):3580–3586
Giglio MC, Celentano V, Tarquini R, Luglio G, De Palma GD, Bucci L (2015) Conversion during laparoscopic colorectal resections: a complication or a drawback? A systematic review and meta-analysis of short-term outcomes. Int J Colorectal Dis 30(11):1445–1455
Mino JS, Gandhi NS, Stocchi LL, Baker ME, Liu X, Remzi FH et al (2015) Preoperative risk factors and radiographic findings predictive of laparoscopic conversion to open procedures in Crohn’s disease. J Gastrointest Surg 19(6):1007–1014
Schmidt CM, Talamini MA, Kaufman HS, Lilliemoe KD, Learn P, Bayless T (2001) Laparoscopic surgery for Crohn’s disease: reasons for conversion. Ann Surg 233(6):733–739
Li J, Guo H, Guan XD, Cai CN, Yang LK, Li YC et al (2015) The impact of laparoscopic converted to open colectomy on short-term and oncologic outcomes for colon cancer. J Gastrointest Surg 19(2):335–343
Sujatha-Bhaskar S, Alizadeh RF, Inaba CS, Koh CY, Jafari MD, Mills SD et al (2018) Respiratory complications after colonic procedures in chronic obstructive pulmonary disease: does laparoscopy offer a benefit? Surg Endosc 32(3):1280–1285
McKenna NP, Habermann EB, Zielinski MD, Lightner AL, Mathis KL (2019) Body mass index: implications on disease severity and postoperative complications in patients with Crohn’s disease undergoing abdominal surgery. Surgery 166(4):703–708
He Y, Wang J, Bian H, Deng X, Wang Z (2017) BMI as a predictor for perioperative outcome of laparoscopic colorectal surgery: a pooled analysis of comparative studies. Dis Colon Rectum 60(4):433–445
Abd El Aziz MA, Grass F, Behm KT, Shawki S, D’Angelo AL, Mathis KL et al (2020) Trends of complications and innovative techniques’ utilization for colectomies in the United States. Updates Surg. https://doi.org/10.1007/s13304-020-00862-y
Abd El Aziz MA, Grass F, Perry W, Behm KT, Shawki SF, Larson DW et al (2020) Colectomy for patients with super obesity: current practice and surgical morbidity in the United States. Surg Obesity Relat Dis 16:1764
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abd El Aziz, M.A., Grass, F., Behm, K.T. et al. Trends and consequences of surgical conversion in the United States. Surg Endosc 36, 82–90 (2022). https://doi.org/10.1007/s00464-020-08240-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08240-w