Abstract
Background
Gastrointestinal endoscopy (GIE) is not routinely accessible in many parts of rural Africa. As surgical training expands and technology progresses, the capacity to deliver endoscopic care to patients improves. We aimed to describe the current burden of gastrointestinal (GI) disease undergoing GIE by examining the experience of surgical training related to GIE.
Methods
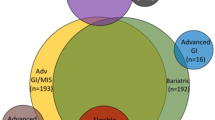
A retrospective review was conducted on GIE procedures performed by trainees with complete case logs during 5-year general surgery training at Pan-African Academy of Christian Surgeons (PAACS) sites. Cases were classified according to diagnosis and/or indication, anatomic location, intervention, adverse events, and outcomes. Comparisons were performed by institutional location and case volumes. Analysis was performed for trainee self-reported autonomy by post-graduate year and case volume experience.
Results
Twenty trainees performed a total of 2181 endoscopic procedures. More upper endoscopies (N = 1,853) were performed than lower endoscopies (N = 325). Of all procedures, 546 (26.7%) involved a cancer or mass, 267 (12.2%) involved a report of blood loss, and 452 (20.7%) reported pain as a component of the diagnosis. Interventions beyond biopsy were reported in 555 (25%) procedures. Esophageal indications predominated the upper endoscopies, particularly esophageal cancer. Trainees in high-volume centers and in East Africa performed more interventional endoscopy and procedures focused on esophageal cancer. Procedure logs documented adverse events in 39 cases (1.8% of all procedures), including 16 patients (0.8%) who died within 30 days of the procedure. Self-reported autonomy improved with both increased endoscopy experience and post-graduate year.
Conclusions
GIE is an appropriate component of general surgery residency training in Africa, and adequate training can be provided, particularly in upper GI endoscopy, and includes a wide variety of endoscopic therapeutic interventions.

Similar content being viewed by others
References
Mandeville KL, Krabshuis J, Ladep NG, Mulder CJ, Quigley EM, Khan SA (2009) Gastroenterology in developing countries: issues and advances. World J Gastroenterol 15:2839
Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, Conteh L, Dare AJ, Davies J (2015) Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 386:569–624
Hassan C, Aabakken L, Ebigbo A, Karstensen JG, Guy C, Dinis-Ribeiro M, Le Moine O, Vilmann P, Ponchon T (2018) Partnership with African countries: European society of gastrointestinal endoscopy (ESGE)–position statement. Endosc Int Open 6:E1247–E1255
Perl D, Leddin D, Bizos D, Veitch A, N’Dow J, Bush-Goddard S, Njie R, Lemoine M, Anderson ST, Igoe J (2016) Endoscopic capacity in west Africa. African Health Sci 16:329–338
Stewart BT, Groen RS, Kamara TB, Kwon S, Kingham TP, Kushner AL (2016) Rectal bleeding and endoscopy need in Sierra Leone: results of a nationwide, cluster-randomized, community-based survey. Int J Colorectal Dis 31:939–941
Raykar NP, Yorlets RR, Liu C, Goldman R, Greenberg SL, Kotagal M, Farmer PE, Meara JG, Roy N, Gillies RD (2016) The how project: understanding contextual challenges to global surgical care provision in low-resource settings. BMJ Global Health 1:e000075
Van Essen C, Steffes BC, Thelander K, Akinyi B, Li H-F, Tarpley MJ (2019) Increasing and retaining African surgeons working in rural hospitals: an analysis of PAACS surgeons with twenty-year program follow-up. World J Surg 43:75–86
Agyei-Nkansah A, Amoako Duah MA (2019) Indications and findings of upper gastrointestinal endoscopy in patients presenting to a district hospital, Ghana. Pan Afr Med J. https://doi.org/10.11604/pamj.2019.34.82.18002
Alatise OI, Aderibigbe AS, Adisa AO, Adekanle O, Agbakwuru AE, Arigbabu AO (2014) Management of overt upper gastrointestinal bleeding in a low resource setting: a real world report from Nigeria. BMC Gastroenterol 14:210
Alema O, Martin D, Okello T (2012) Endoscopic findings in upper gastrointestinal bleeding patients at lacor hospital, northern Uganda. African Health Sci 12:518–521
Qureshi J, Mulima G, Tamimi S, Klackenberg H, Andren-Sandberg Ů, Charles A, Shores C (2014) Epidemiology of upper gastrointestinal bleeding in a sub saharan African tertiary hospital. J Surg Res 186:553
Sibomana I, Niyongombwa I, Dusabejambo V, Kiswezi A (2019) Lower gastrointestinal bleeding at a referral hospital in Kigali, Rwanda: clinical, colonoscopic and pathologic profiles. East Cent Afr J Surg 24:101–104
Bane A, Bekele A (2012) Management of gastrointestinal foreign bodies using flexible endoscopy: an experience from addis Ababa, Ethiopia. East Cent Afr J Surg 17:32–38
Kelly P, Katema M, Amadi B, Zimba L, Aparicio S, Mudenda V, Baboo KS, Zulu I (2008) Gastrointestinal pathology in the university teaching hospital, Lusaka, Zambia: review of endoscopic and pathology records. Trans R Soc Trop Med Hyg 102:194–199
Parker RK, Dawsey SM, Abnet CC, White RE (2010) Frequent occurrence of esophageal cancer in young people in western Kenya. Dis Esophagus 23:128–135
Parker RK, Ranketi SS, McNelly C, Ongondi M, Topazian HM, Dawsey SM, Murphy GA, White RE, Mwachiro M (2018) Colorectal cancer is increasing in rural Kenya: challenges and perspectives. Gastrointest Endosc 89:1234–1237
Mchembe MD, Rambau PF, Chalya PL, Jaka H, Koy M, Mahalu W (2013) Endoscopic and clinicopathological patterns of esophageal cancer in Tanzania: experiences from two tertiary health institutions. World J Surg Oncol 11:257
Nwokediuko SC, Ijoma U, Obienu O, Picardo N (2012) Time trends of upper gastrointestinal diseases in Nigeria. Annal Gastroenterol 25:52
Ooko PB, Sirera B, Saruni S, Topazian HM, White R (2015) Pattern of adult intestinal obstruction at Tenwek hospital, in south-western Kenya. Pan Afr Med J. https://doi.org/10.11604/pamj.2015.20.31.5830
Raveenthiran V, Madiba T, Atamanalp S, De U (2010) Volvulus of the sigmoid colon. Colorectal Dis 12:e1–e17
Kayamba V (2019) Oesophageal cancer hotspots in Africa. Lancet Gastroenterol Hepatol 4:818–820
Abnet CC, Arnold M, Wei W-Q (2018) Epidemiology of esophageal squamous cell carcinoma. Gastroenterology 154:360–373
Missalek W, Jones F, Mmuni K, Cutinha P (1991) Value of fibreoptic oesophago-gastro-duodenoscopy: experience with 4000 procedures at kilimanjaro christian medical centre, Moshi, Tanzania. Trop Doct 21:165–168
Kamdem J, Palmer D, Barrier C, Bardin R, Brown JA, Topazian M (2018) Diagnostic yield of gastrointestinal endoscopy in north west region cameroon and trends in diagnosis over time. Pan Afr Med J 29:1–5
Mothes H, Chagaluka G, Chiwewe D, Malunga M, Mwatibu B, Wilhelm T, Settmacher U (2009) Do patients in rural malawi benefit from upper gastrointestinal endoscopy? Trop Doct 39:73–76
Kayamba V, Sinkala E, Mwanamakondo S, Soko R, Kawimbe B, Amadi B, Zulu I, Nzaisenga J-B, Banda T, Mumbwe C (2015) Trends in upper gastrointestinal diagnosis over four decades in Lusaka, Zambia: a retrospective analysis of endoscopic findings. BMC Gastroenterol 15:127
Galukande M, Luboga S, Elobu E (2013) Challenges facing surgical training in the great lakes region in sub-saharan Africa: a review article. East Cent Afr J Surg 18:3–11
Parker RK, Topazian HM, Ndegwa W, Chesang P, Strain S, Thelander K, Parker AS, Riviello R (2020) Surgical training throughout Africa: a review of operative case volumes at multiple training centers. World J Surg. https://doi.org/10.1007/s00268-020-05463-9
Parker RK, Topazian HM, Parker AS, Mwachiro MM, Strain S, White RE, Thelander K, Riviello R (2020) Operative case volume minimums necessary for surgical training throughout rural Africa. World J Surg. https://doi.org/10.1007/s00268-020-05609-9
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A, Petersen BT, Petrini JL (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
George BC, Teitelbaum EN, Meyerson SL, Schuller MC, DaRosa DA, Petrusa ER, Petito LC, Fryer JP (2014) Reliability, validity, and feasibility of the Zwisch scale for the assessment of intraoperative performance. J Surg Educ 71:e90–e96
White RE, Parker RK, Fitzwater JW, Kasepoi Z, Topazian M (2009) Stents as sole therapy for oesophageal cancer: a prospective analysis of outcomes after placement. Lancet Oncol 10:240–246
Peery AF, Crockett SD, Murphy CC, Lund JL, Dellon ES, Williams JL, Jensen ET, Shaheen NJ, Barritt AS, Lieber SR (2019) Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology 156(254–272):e211
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. A Cancer J Clin 68:394–424
Cortez AR, Winer LK, Kassam AF, Hanseman DJ, Kuethe JW, Quillin RC, Potts JR (2019) See none, do some teach none: an analysis of the contemporary operative experience as nonprimary surgeon. J Surg Educ. https://doi.org/10.1016/j.jsurg.2019.05.007
Harrington CM, Kavanagh DO, Ryan D, Dicker P, Lonergan PE, Traynor O, Tierney S (2017) Objective scoring of an electronic surgical logbook: analysis of impact and observations within a surgical training body. Am J Surg 214:962–968
Jones DB, Hunter JG, Townsend CM, Minter RM, Roberts PL, Brethauer S, Soper NJ (2017) SAGES rebuttal. Gastrointest Endosc 86:751–754
ABS (2018) Booklet of Info - surgery. American board of surgery, Philadelphia, PA
Faulx AL, Lightdale JR, Acosta RD, Agrawal D, Bruining DH, Chandrasekhara V, Eloubeidi MA, Gurudu SR, Kelsey L, Khashab MA (2017) Guidelines for privileging, credentialing, and proctoring to perform GI endoscopy. Gastrointest Endosc 85:273–281
May FP, Anandasabapathy S (2019) Colon cancer in Africa: primetime for screening? Gastrointest Endosc 89:1238–1240
Chao TE, Rosenberg J, Patel P, Riviello R, Weintraub R (2011) Surgery at AIC kijabe hospital in rural Kenya. Population (thousands) 41:610
White RE, Parker RK (2017) Delivery of subspecialty surgical care in low-resource settings. In: Park AaP, Raymond (eds) Global surgery, Springer, pp. 69–107
Waweru J, Ojuka D, Jani P, Kiraitu W, Onyango S, Okumu W (2018) The practice of interventional gastrointestinal endoscopy at a tertiary referral hospital. Annal Afr Surg. https://doi.org/10.4314/aas.v15i1.7
Cooper MA, Tinmouth JM, Yong E, Walsh CM, Carnahan H, Grover SC, Ritvo P (2014) Surgical residents’ perceptions on learning gastrointestinal endoscopy: more hours and more standardization wanted. J Surg Educ 71:899–905
Asombang AW, Turner-Moss E, Seetharam A, Kelly P (2013) Gastroenterology training in a resource-limited setting: zambia, Southern Africa. World J Gastroenterol 19:3996
Wilhelm T, Mothes H, Chiwewe D, Mwatibu B, Kähler G (2012) Gastrointestinal endoscopy in a low budget context: delegating EGD to non-physician clinicians in Malawi can be feasible and safe. Endoscopy 44:174–176
Pearl J, Fellinger E, Dunkin B, Pauli E, Trus T, Marks J, Fanelli R, Meara M, Stefanidis D, Richardson W (2016) Guidelines for privileging and credentialing physicians in gastrointestinal endoscopy. Surg Endosc 30:3184–3190
Parker RK, Oloo M, Mogambi FC, White RE, Parker AS (2020) Operative self-confidence, hesitation, and ability assessment of surgical trainees in rural Kenya. J Surg Res 258:137–144
Funding
The authors wish to acknowledge the SAGES Education & Research Foundation for the grant, “Improving Surgical and Endoscopy Access and Training in East Africa,” which allowed for the completion of this project.
Author information
Authors and Affiliations
Contributions
All authors contributed to meet all four requirements of ICJME recommendations. Robert Parker, Hillary Topazian, Michael Mwachiro, Richard Davis, Albert Nyanga, Zachary Connor, Stephen Burgert, and Mark Topazian contributed to the concept and design of the project or to data acquisition, analysis, and interpretation. Robert Parker drafted the initial manuscript with Hillary Topazian, Michael Mwachiro, and Mark Topazian and each author Robert Parker, Hillary Topazian, Michael Mwachiro, Richard Davis, Albert Nyanga, Zachary Connor, Stephen Burgert, and Mark Topazian offered critical revisions for important intellectual content. All authors approved the final manuscript and accept responsibility. The corresponding author, Robert Parker, confirms that he had full access to the data and the final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Disclosure
The authors, Robert Parker, Michael Mwachiro, Hillary Topazian, Richard Davis, Albert Nyanga, Zachary O’Connor, Stephen Burgert, and Mark Topazian have no conflicts of interest or financial ties to disclose.
Ethical approval
The study received ethical approval from the Tenwek Hospital Institutional Ethics Review Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parker, R.K., Mwachiro, M.M., Topazian, H.M. et al. Gastrointestinal endoscopy experience of surgical trainees throughout rural Africa. Surg Endosc 35, 6708–6716 (2021). https://doi.org/10.1007/s00464-020-08174-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08174-3