Abstract
Background
sophageal cancer has a low incidence, and the anatomy is difficult to understand during esophagectomy. This necessitates a precise and lengthy operation. Therefore, the establishment of a training system in esophageal surgery is of critical importance. In this study, we compared the short-term outcomes of minimally invasive esophagectomy (MIE) performed by consultants versus trainees and explored the factors that impacted the thoracic operation time for each group.
Methods
We have introduced standardized MIE surgical techniques to our trainees in 2016. Our procedure consists of a laparoscopic phase and a thoracoscopic phase and is systematically designed to be learned in a step-by-step manner in each phase. We retrospectively identified 308 patients who underwent MIE from April 2016 to April 2018. The patients were divided into those who underwent MIE by consultants and those who underwent MIE by trainees. The preoperative background factors, operation-related factors, and postoperative complications were compared between the two groups. We also assessed the association between a prolonged thoracic operation time and tumor-and patient-related factors in each of the consults and trainees.
Results
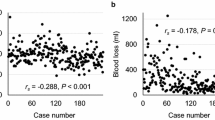
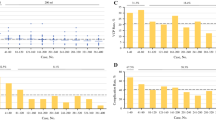
Significantly more patients had stage ≥ III cancer in the consultant than trainee group. However, the postoperative complications were comparable, specifically pneumonia (11% vs. 18%), anastomotic leakage (11% vs. 13%), and mortality (0.6% vs. 1.3%). There was no significant difference in the lymph node yield (20 vs. 17) or R0 resection rate (94% vs. 91%) between the two groups. However, the trainees had a significantly longer thoracic operation time (143 ± 34 vs. 190 ± 28 min) and significantly greater blood loss (93 vs. 183 ml). Oncological factors were correlated with a prolonged thoracic operation time in the consultants, but not in the trainees.
Conclusions
Under standardized surgical management using a stepwise educational program, performance of MIE by trainees has no impact on short-term outcomes.
Similar content being viewed by others
References
Cooper JS, Guo MD, Herskovic A, Macdonald JS, Martenson JA Jr, Al-Sarraf M, Byhardt R, Russell AH, Beitler JJ, Spencer S, Asbell SO, Graham MV, Leichman LL (1999) Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85–01) Radiation Therapy Oncology Group. Jama 281:1623–1627
Shitara K, Muro K (2009) Chemoradiotherapy for treatment of esophageal cancer in Japan: current status and perspectives. Gastrointest Cancer Res: GCR 3:66–72
Lagergren J, Smyth E, Cunningham D, Lagergren P (2017) Oesophageal cancer. Lancet (London, England) 390:2383–2396
Fujita H, Kakegawa T, Yamana H, Shima I, Toh Y, Tomita Y, Fujii T, Yamasaki K, Higaki K, Noake T et al (1995) Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg 222:654–662
Masuda M, Okumura M, Doki Y, Endo S, Hirata Y, Kobayashi J, Kuwano H, Motomura N, Nishida H, Saiki Y, Saito A, Shimizu H, Tanaka F, Tanemoto K, Toh Y, Tsukihara H, Wakui S, Yokomise H (2016) Thoracic and cardiovascular surgery in Japan during 2014: annual report by the japanese association for thoracic surgery. General Thorac Cardiovas Surg 64:665–697
Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH, Hollmann MW, de Lange ES, Bonjer HJ, van der Peet DL, Cuesta MA (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet (London, England) 379:1887–1892
Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, Tomita N, Nakagoe T, Shimada M, Sugihara K, Mori M (2014) A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg 260:259–266
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J Clin 68:394–424
Takeno S, Tanoue Y, Hamada R, Kawano F, Tashiro K, Wada T, Ikenoue M, Nanashima A, Nakamura K (2019) Utility of thoracic cage width in assessing surgical difficulty of minimally invasive esophagectomy in left lateral decubitus position. Surgical endoscopy
Okamura A, Watanabe M, Mine S, Nishida K, Imamura Y, Kurogochi T, Kitagawa Y, Sano T (2016) Factors influencing difficulty of the thoracic procedure in minimally invasive esophagectomy. Surg Endosc 30:4279–4285
Uchihara T, Yoshida N, Baba Y, Nakashima Y, Kimura Y, Saeki H, Takeno S, Sadanaga N, Ikebe M, Morita M, Toh Y, Nanashima A, Maehara Y, Baba H (2020) Esophageal position affects short-term outcomes after minimally invasive esophagectomy: a retrospective multicenter study. World journal of surgery 44:831–837
Wagner JP, Lewis CE, Tillou A, Agopian VG, Quach C, Donahue TR, Hines OJ (2018) Use of entrustable professional activities in the assessment of surgical resident competency. JAMA Surg 153:335–343
Blencowe NS, Parsons BA, Hollowood AD (2011) Effects of changing work patterns on general surgical training over the last decade. Postgrad Med J 87:795–799
Lewis FR, Klingensmith ME (2012) Issues in general surgery residency training–2012. Ann Surg 256:553–559
Phillips AW, Madhavan A (2013) A critical evaluation of the intercollegiate surgical curriculum and comparison with its predecessor the “Calman” curriculum. J Surg Educ 70:557–562
Sonnadara RR, Mui C, McQueen S, Mironova P, Nousiainen M, Safir O, Kraemer W, Ferguson P, Alman B, Reznick R (2014) Reflections on competency-based education and training for surgical residents. J Surg Educ 71:151–158
Phillips AW, Dent B, Navidi M, Immanuel A, Griffin SM (2018) Trainee involvement in ivor lewis esophagectomy does not negatively impact outcomes. Ann Surg 267:94–98
Handagala SD, Addae-Boateng E, Beggs D, Duffy JP, Martin-Ucar AE (2012) Early outcomes of surgery for oesophageal cancer in a thoracic regional unit. Can we maintain training without compromising results? Eur J Cardio-Thorac Surg: Off J Eur Assoc Cardio-Thoracic Surgery 41:31-34; discussion 34-35
Daiko H, Fujita T (2015) Laparoscopic assisted versus open gastric pull-up following thoracoscopic esophagectomy: a cohort study. Int J Surg (London, England) 19:61–66
Daiko H, Nishimura M (2012) A pilot study of the technical and oncologic feasibility of thoracoscopic esophagectomy with extended lymph node dissection in the prone position for clinical stage I thoracic esophageal carcinoma. Surg Endosc 26:673–680
Fujiwara H, Kanamori J, Nakajima Y, Kawano T, Miura A, Fujita T, Akita K, Daiko H (2019) An anatomical hypothesis: a "concentric-structured model" for the theoretical understanding of the surgical anatomy in the upper mediastinum required for esophagectomy with radical mediastinal lymph node dissection. Diseases of the esophagus: official journal of the International Society for Diseases of the Esophagus 32
Baron R, Sujendran V, Maynard N (2008) Should oesophagectomies be performed by trainees? The experience from a single teaching centre under the supervision of one surgeon. Ann Royal Coll Surg England 90:305–309
Park A, Witzke D, Donnelly M (2002) Ongoing deficits in resident training for minimally invasive surgery. J Gastrointest Surg: Off J Soc Surg Aliment Tract 6:501-507; discussion 507-509
Ogiso S, Yamaguchi T, Hata H, Kuroyanagi H, Sakai Y (2010) Introduction of laparoscopic low anterior resection for rectal cancer early during residency: a single institutional study on short-term outcomes. Surg Endosc 24:2822–2829
Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE (2002) Hospital volume and surgical mortality in the United States. New England J Med 346:1128–1137
Fuchs HF, Harnsberger CR, Broderick RC, Chang DC, Sandler BJ, Jacobsen GR, Bouvet M, Horgan S (2017) Mortality after esophagectomy is heavily impacted by center volume: retrospective analysis of the Nationwide Inpatient Sample. Surg Endosc 31:2491–2497
Yoshida N, Baba Y, Shigaki H, Shiraishi S, Harada K, Watanabe M, Iwatsuki M, Kurashige J, Sakamoto Y, Miyamoto Y, Ishimoto T, Kosumi K, Tokunaga R, Yamashita Y, Baba H (2016) Effect of esophagus position on surgical difficulty and postoperative morbidities after thoracoscopic esophagectomy. Semin Thorac Cardiovas Surg 28:172–179
Otsubo D, Nakamura T, Yamamoto M, Kanaji S, Kanemitsu K, Yamashita K, Imanishi T, Oshikiri T, Sumi Y, Suzuki S, Kuroda D, Kakeji Y (2017) Prone position in thoracoscopic esophagectomy improves postoperative oxygenation and reduces pulmonary complications. Surg Endosc 31:1136–1141
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Koshiro Ishiyama, Daisuke Kurita, Junya Oguma, Hisashi Fujiwara, Takeo Fujita, Hitoshi Katai, and Hiroyuki Daiko have no conflicts of interest or financial relationships to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ishiyama, K., Fujita, T., Fujiwara, H. et al. Does staged surgical training for minimally invasive esophagectomy have an impact on short-term outcomes?. Surg Endosc 35, 6251–6258 (2021). https://doi.org/10.1007/s00464-020-08125-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08125-y