Abstract
Background
Malignant biliary obstruction secondary to metastatic cancer is associated with poor prognosis. To the best of our knowledge, no previous study has investigated long-term survival and associated prognostic factors after biliary endoscopic retrograde cholangiopancreatography (ERCP) drainage for obstruction jaundice secondary to various types of metastatic cancer.
Methods
This retrospective study included 60 patients who underwent biliary ERCP drainage for obstructive jaundice secondary to metastatic cancer at two hospitals during the period from November 2012 to December 2019. Multivariate analysis was conducted to identify independent prognostic factors.
Results
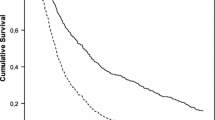
Biliary drainage was successfully achieved in 55 (91.7%) patients, 37 of whom received subsequent treatment. Overall median survival time was 133 days after stent placement. The overall survival (OS) rates after ERCP drainage were significantly better in the post-drainage treatment group than in the post-drainage untreated group (239 days vs. 45 days, p < 0.001). Good ECOG performance status before drainage, albumin level ≥ 35 g/L, successful drainage, absence of ascites, and post-drainage treatment were identified as factors of improved survival in univariate analysis. ECOG performance status and post-drainage treatment were independent predictors of OS in multivariate analysis.
Conclusions
We showed that stent placement with ERCP was a safe and effective treatment method for patients with malignant biliary obstruction caused by metastatic cancer and may be preferred over percutaneous transhepatic biliary drainage. Post-drainage treatment and a good ECOG performance status were predictors of better prognosis.



Similar content being viewed by others
References
Migita K, Watanabe A, Yoshioka T et al (2009) Clinical outcome of malignant biliary obstruction caused by metastatic gastric cancer. World J Surg 33:2396–2402
Gwon DI, Ko GY, Sung KB et al (2012) Clinical outcomes after percutaneous biliary interventions in patients with malignant biliary obstruction caused by metastatic gastric cancer. Acta Radiol 53:422–429
Hong HP, Seo TS, Cha IH et al (2013) Percutaneous placement of self-expandable metallic stents in patients with obstructive jaundice secondary to metastatic gastric cancer after gastrectomy. Korean J Radiol 14:789–796
Sellier F, Bories E, Sibertin-Blanc C et al (2018) Clinical outcome after biliary drainage for metastatic colorectal cancer: survival analysis and prognostic factors. Dig Liver Dis 50:189–194
Nichols SD, Albert S, Shirley L et al (2014) Outcomes in patients with obstructive jaundice from metastatic colorectal cancer and implications for management. J Gastrointest Surg 18:2186–2191
Chaudhari D, Khanna A, Goenka P, Young M (2014) Lung carcinoma presenting as an obstructive jaundice: case series with literature review. J Gastrointest Cancer 45(Suppl 1):66–70
Nakazawa K, Tamura T, Sato S et al (2013) Obstructive jaundice as recurrence of lung adenocarcinoma. J Gastrointest Cancer 44:248–249
Yu CZ, Yu CH, Nai C, Tian J (2015) A presenting with obstructive jaundice in pulmonary adenocarcinoma: a case report. Int J Clin Exp Med 8:11613–11616
Lin Y, Wong SI, Wang Y et al (2019) Periampullary Metastases from breast cancer: a case report and literature review. Case Rep Oncol Med 2019:1–6
Karakatsanis A, Vezakis A, Fragulidis G et al (2013) Obstructive jaundice due to ampullary metastasis of renal cell carcinoma. World J Surg Oncol 11:262
Takasaki Y, Irisawa A, Shibukawa G et al (2018) A case of obstructive jaundice caused by metastasis of ovarian cancer to the duodenal major papilla. Clin Med Insights Case Rep 11:1–4
Ahmmad E, Abdulkarim AS, Dirweesh A (2019) Peri-ampullary metastasis from endometrial adenocarcinoma: a rare etiology of obstructive jaundice. Gastroenterology Res 12:37–39
Dumonceau JM, Tringali A, Papanikolaou IS et al (2018) Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline—Updated October 2017. Endoscopy 50:910–930
Afshar M, Khanom K, Ma YT, Punia P (2014) Biliary stenting in advanced malignancy: an analysis of predictive factors for survival. Cancer Manag Res 6:475–479
Kasuga A, Ishii H, Ozaka M et al (2012) Clinical outcome of biliary drainage for obstructive jaundice caused by colorectal and gastric cancers. Jpn J Clin Oncol 42:1161–1167
Meller MT, Arts GR, Dean JR (2010) Outcomes in percutaneous stenting of non-hepato-biliary/pancreatic malignant jaundice. Eur J Cancer Care (Engl) 19:664–668
Inamdar S, Slattery E, Bhalla R et al (2016) Comparison of adverse events for endoscopic vs percutaneous biliary drainage in the treatment of malignant biliary tract obstruction in an inpatient national cohort. JAMA Oncol 2:112–117
Wang L, Lin N, Xin F et al (2019) A systematic review of the comparison of the incidence of seeding metastasis between endoscopic biliary drainage and percutaneous transhepatic biliary drainage for resectable malignant biliary obstruction. World J Surg Oncol 17:116
Chapman WC, Sharp KW, Weaver F, Sawyers JL (1989) Tumor seeding from percutaneous biliary catheters. Ann Surg 209:708–713
Teoh AYB, Dhir V, Kida M et al (2018) Consensus guidelines on the optimal management in interventional EUS procedures: results from the Asian EUS group RAND/UCLA expert panel. Gut 67:1209–1228
Makino T, Fujitani K, Tsujinaka T et al (2008) Role of percutaneous transhepatic biliary drainage in patients with obstructive jaundice caused by local recurrence of gastric cancer. Hepatogastroenterology 55:54–57
Wainberg ZA, Feeney K, Lee MA et al (2020) Meta-analysis examining overall survival in patients with pancreatic cancer treated with second-line 5-fluorouracil and oxaliplatin-based therapy after failing first-line gemcitabine-containing therapy: effect of performance status and comparison with other regimens. BMC Cancer 20:633
Sargent DJ, Kohne CH, Sanoff HK et al (2009) Pooled safety and efficacy analysis examining the effect of performance status on outcomes in nine first-line treatment trials using individual data from patients with metastatic colorectal cancer. J Clin Oncol 27:1948–1955
Lee J, Lim T, Uhm JE et al (2007) Prognostic model to predict survival following first-line chemotherapy in patients with metastatic gastric adenocarcinoma. Ann Oncol 18:886–891
Tringali A, Hassan C, Rota M et al (2018) Covered vs. uncovered self-expandable metal stents for malignant distal biliary strictures: a systematic review and meta-analysis. Endoscopy 50:631–641
Almadi MA, Barkun A, Martel M (2017) Plastic vs. Self-expandable metal stents for palliation in malignant biliary obstruction: a series of meta-analyses. Am J Gastroenterol 112:260–273
Acknowledgements
We appreciate the hard work of the colleagues at the database center of two hospitals who helped us reserve and search the relative data. Furthermore, we thank the Enago editing service.
Funding
This study was funded by Beijing Municipal Administration of Hospitals Incubating Program (Grant Number PX 2,020,047).
Author information
Authors and Affiliations
Contributions
As the leading principle investigator of the study, Professor WQ, LX contributed significantly to the study design and final approval of the article. YP contributed to data analysis and drafting of the manuscript. ZL, LSJ were responsible for analysis and interpretation of the data and critical revision of the article for important intellectual content. All authors provided significant input to the paper by means of revisions and all have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Disclosures
Drs. Peng Yuan, Lei Zhang, Shijie Li, Xun Li, Qi Wu have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yuan, P., Zhang, L., Li, S. et al. Clinical results after biliary drainage by endoscopic retrograde cholangiopancreatography for analysis of metastatic cancer survival and prognostic factors. Surg Endosc 35, 6220–6226 (2021). https://doi.org/10.1007/s00464-020-08121-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08121-2