Abstract
Background
Anastomotic leak still represents the most feared surgical complication following colorectal resection and is associated with high morbidity and mortality rates. The aim of this study is to assess the feasibility and safety of laparoscopic reoperation for symptomatic anastomotic leak (AL) after laparoscopic right colectomy with mechanical intracorporeal anastomosis (IA).
Methods
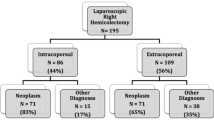
From January 2012 to December 2019, 428 consecutive laparoscopic right colectomy with IA were performed. Overall symptomatic AL rate requiring reoperation was 5.8% (26/428). Data on patient demographics as well as operative findings, time elapsed from primary surgery and from the onset of symptoms of anastomotic leak, time and duration of re-laparoscopy, ICU stay, morbidity, mortality rate, length of hospital stay and readmission, were all retrospectively reviewed.
Results
Laparoscopic approach was attempted in 23 (88.4%) hemodynamically stable patients. Conversion rate was 21.4%. Reasons for conversion were gross fecal peritonitis (n = 2), colonic ischemia (n = 1), severe bowel distension (n = 2). Eighteen (78.2%) patients underwent successfully laparoscopic (LPS) reoperation. A repair of the anastomotic defect was done in 11 (61.1%) patients, while in 7 patients the intracorporeal mechanical anastomosis was refashioned. A diverting ileostomy was done in 22.2% of cases (n = 4). A second reoperation for leak persistence was necessary in two cases (11.1%). Median (range) length of postoperative hospital stay from re-laparoscopy was 15.5 (9–53) days. Overall morbidity rate was 38.7%. Mortality rate was 5.5% (n = 1)
Conclusion
laparoscopic re-intervention for the treatment of anastomotic leak following LPS right colectomy with intracorporeal anastomosis in hemodynamically stable and highly selected patients in the experienced hands of dedicated laparoscopic surgeons, is a safe option with acceptable morbidity and mortality rate.
Similar content being viewed by others
References
Soeters PB, de Zoete JP, Dejong CH, Williams NS, Baeten CG (2002) Colorectal surgery and anastomotic leakage. Dig Surg 19:150–155. https://doi.org/10.1159/0000520312
Buchs NC, Gervaz P, Secic M, Bucher P, Mugnier-Konrad B, Morel P (2008) Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis 23:265–270. https://doi.org/10.1007/s00384-007-0399-3
Joh YG, Kim SH, Hahn KY, Stulberg J, Chung CS, Lee DK (2009) Anastomotic leakage after laparoscopic proctectomy can be managed by a minimally invasive approach. Dis Colon Rectum 52:91–96. https://doi.org/10.1007/DCR.0b013e3181973d7f
Vennix S, Abegg R, Bakker OJ, van den Boezem PB, Brokelman WJ, Sietses C, Bosscha K, Lips DJ, Prins HA (2014) Surgical re-interventions following colorectal surgery: open versus laparoscopic management of anastomotic leakage. J Laparoendosc Adv Surg Tech A 23:739–774. https://doi.org/10.1089/lap.2012.0440
Wind J, Koopman AG, van Berge Henegouwen MI, Slors JF, Gouma DJ, Bemelman WA (2007) Laparoscopic re-intervention for anastomotic leakage after primary laparoscopic colorectal surgery. Br J Surg 94:1562–1566. https://doi.org/10.1002/BJS.5892
Chang KH, Bourke MG, Kavanagh DO, Neary PC, O’Riordan JM (2016) A systematic review of the role of re-laparoscopy in the management of complications following laparoscopic colorectal surgery. Surgeon 14:287–2939. https://doi.org/10.1016/j.surge.2015.12.003
Wright DB, Koh CE, Solomon MJ (2017) Systematic review of the feasibility of laparoscopic reoperation for early postoperative com-plications following colorectal surgery. Br J Surg 104:337–346. https://doi.org/10.1002/bjs.10469
Eriksen JR, Ovesen H (2018) Gogenur I (2018) Short and long-term outcomes after colorectal anastomotic leakage is affected by surgical approach at reoperation. Int J Colorectal Dis 33:1097–1105. https://doi.org/10.1007/s00384-018-3079-6,May12
Li YW, Lian P, Huang B, Zheng HT, Wang MH, Gu WL, Li XX, Xu Y, Cai SJ (2017) Very early colorectal anastomotic leakage within 5 post-operative days: a more severe subtype needs relaparatomy. Sci Rep 7:39936. https://doi.org/10.1038/srep39936
Vignali A, Elmore U, Lemma M, Guarnieri G, Radaelli G (2018) Rosati R (2018) Intracorporeal versus extracorporeal anastomoses following laparoscopic right colectomy in obese patients: a case-matched study. Dig Surg 35:236–242. https://doi.org/10.1159/000479241
Cuccurullo D, Pirozzi F, Sciuto A, Bracale U, La Barbera C, Galante F, Corcione F (2015) Re-laparoscopy for management of postoperative complications following colorectal surgery: ten years experience in a single center. Surg Endosc 29:1795–1803. https://doi.org/10.1007/s00464-014-3862-6
Marano A, Giuffrida MC, Giraudo G, Pellegrino L, Borghi F (2016) Management of peritonitis after minimally invasive colorectal surgery. Can we stick to laparoscopy ? J Laparoendosc Adv Surg Tech 27:342–347. https://doi.org/10.1089/lap.2016.0374
Bakker IS, Grossmann I, Henneman D, Havenga K, Wiggers T (2014) Risk factors for anastomotic leakage and leak-related mortality after colonic cancer surgery in a nationwide audit. BJS 101:424–432. https://doi.org/10.1002/bjs.9395
Garcia-Granero A, Frasson M, Flor-Lorente B, Blanco F, Puga R, Carratalá A, Garcia-Granero E (2013) Procalcitonin and C-reactive protein as early predictors of anastomotic leak in colorectal surgery: a prospective observational study. Dis Colon Rectum. 56:475–483. https://doi.org/10.1097/DCR.0b013e31826ce825
Daams F, Wu Z, Lahaye MJ, Jeekel J, Lange JF (2014) Prediction and diagnosis of colorectal anastomotic leakage: a systematic review of literature. World J Gastrointest Surg 6:14–26. https://doi.org/10.4240/wjgs.v6.i2.14
Cimitan A, Contaldo T, Malaro R, Morpurgo E (2016) The role of laparoscopy in the treatment of anastomotic leak after minimally invasive colorectal resection for cancer. Surg Laparosc Endosc Percutan Tech 26:e80. https://doi.org/10.1097/SLE.0000000000000301
Thornton M, Joshi H, Vimalachandran C, Heath R, Carter P, Gur U, Rooney P (2011) Management and outcome of colorectal anastomotic leaks. Int J Colorectal Dis 26:313–320. https://doi.org/10.1007/s00384-010-1094-3
Fraccalvieri D, Biondo S, Saez J, Millan M, Kreisler E, Golda T, Frago R, Miguel B (2012) Management of colorectal anastomotic leakage: differences between salvage and anastomotic takedown. Am J Surg 204:671–676. https://doi.org/10.1016/j.amjsurg.2010.04.022
Kwak JM, Kim SH, Son DN, Kim J, Lee SI, Min BW, Um JW, Moon HY (2011) The role of laparoscopic approach for anastomotic leakage after minimally invasive surgery for colorectal cancer. J Laparoendosc Adv Surg Tech A 21:29–33. https://doi.org/10.1089/lap.2010.0407
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Professor Andrea Vignali, Drs. Ugo Elmore, Francesca Aleotti, Roberto Delpini, Paolo Parise and Professor Riccardo Rosati declare that they have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vignali, A., Elmore, U., Aleotti, F. et al. Re-laparoscopy in the treatment of anastomotic leak following laparoscopic right colectomy with intracorporeal anastomosis. Surg Endosc 35, 6173–6178 (2021). https://doi.org/10.1007/s00464-020-08113-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08113-2