Abstract
Introduction
Venous thromboembolism (VTE) is a significant cause of morbidity and mortality after bariatric surgery. Roughly 80% of VTEs occur post-discharge. The frequency of post-discharge heparin (PDH) prophylaxis use is unknown, and evidence about benefits and risks is limited. We aimed to determine the rate of use of PDH prophylaxis and evaluate its relationship with VTE and bleeding events.
Methods
Using the Truven Health MarketScan® database, we performed a retrospective cohort study (2007–2015) of adult patients who underwent sleeve gastrectomy or gastric bypass. We determined PDH prophylaxis from outpatient pharmacy claims, and post-discharge 90-day VTE and bleeding events from outpatient and inpatient claims. We used propensity score-adjusted regression models to mitigate confounding bias.
Results
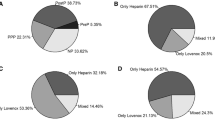
Among 43,493 patients (median age 45 years; 78% women; 77% laparoscopic gastric bypass, 17% laparoscopic sleeve gastrectomy, 6% open gastric bypass), 6% received PDH prophylaxis. Overall, 224 patients (0.52%) experienced VTEs, and 806 patients (1.85%) experienced bleeding. The unadjusted VTE rate did not differ between patients who did and did not receive PDH prophylaxis (0.39% vs. 0.52%, respectively; p = 0.347). The unadjusted bleeding rate was higher for the PDH prophylaxis group (2.74% vs. 1.80%, p < 0.001). In our adjusted analysis, a 23% lower risk of VTE in the PDH prophylaxis group was not statistically significant (odds ratio [OR] 0.77, 95% confidence interval [CI] 0.41 to 1.46), whereas the 47% higher risk of bleeding was statistically significant (OR 1.47, 95% CI 1.14 to 1.88).
Conclusions
PDH prophylaxis after bariatric surgery is uncommon. In our analysis, use was not associated with a lower VTE risk but was associated with a higher bleeding risk.

Similar content being viewed by others
References
Hales CM, Carroll MD, Fryar CD, Ogden CL (2017) Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief 288:1–8
Balla A, Batista Rodríguez G, Corradetti S, Balagué C, Fernández-Ananín S, Targarona EM (2017) Outcomes after bariatric surgery according to large databases: a systematic review. Langenbeck’s Arch Surg 402:885–899
Courcoulas AP, King WC, Belle SH, Berk P, Flum DR, Garcia L, Gourash W, Horlick M, Mitchell JE, Pomp A, Pories WJ, Purnell JQ, Singh A, Spaniolas K, Thirlby R, Wolfe BM, Yanovski SZ (2018) Seven-year weight trajectories and health outcomes in the longitudinal assessment of bariatric surgery (LABS) study. JAMA Surg 153:427–434
Sanni A, Perez S, Medbery R, Urrego HD, McCready C, Toro JP, Patel AD, Lin E, Sweeney JF, Davis SS (2014) Postoperative complications in bariatric surgery using age and BMI stratification: a study using ACS-NSQIP data. Surg Endosc 28(12):3302–3309
Encinosa WE, Bernard DM, Du D, Steiner CA (2009) Recent Improvements in bariatric surgery outcomes. Med Care 47(5):531–535
Agency for Healthcare Research and Quality (AHRQ). Statistical Brief #23. Bariatric surgery utilization and outcomes in 1998 and 2004 (2007). https://www.hcup-us.ahrq.gov/reports/statbriefs/sb23.jsp. Accessed May 22, 2020.
Smith MD, Patterson E, Wahed AS, Belle SH, Berk PD, Courcoulas AP, Dakin GF, Flum DR, Machado L, Mitchell JE, Pender J, Pomp A, Pories W, Ramanathan R, Schrope B, Staten M, Akuenzunkpa U, Wolfe BM (2011) Thirty-day mortality after bariatric surgery: independently adjudicated causes of death in the longitudinal assessment of bariatric surgery. Obes Surg 21:1687–1692
Froehling DA, Daniels PR, Mauck KF, Collazo-Clavell ML, Ashrani AA, Sarr MG, Petterson TM, Bailey KR, Heit JA (2013) Incidence of venous thromboembolism after bariatric surgery: a population-based cohort study. Obes Surg 23:1874–1879
Tagalakis V, Patenaude V, Kahn SR, Suissa S (2013) Incidence of and mortality from venous thromboembolism in a real-world population: the Q-VTE study cohort. Am J Med 126:832.e13–832.e21
Morino M, Toppino M, Forestieri P, Angrisani L, Allaix ME, Scopinaro N (2007) Mortality after bariatric surgery. Ann Surg 246:1002–1009
Jamal MH, Corcelles R, Shimizu H, Kroh M, Safdie FM, Rosenthal R, Brethauer SA, Schauer PR (2015) Thromboembolic events in bariatric surgery: a large multi-institutional referral center experience. Surg Endosc 29:376–380
Finks JF, English WJ, Carlin AM, Krause KR, Share DA, Banerjee M, Birkmeyer JD, Birkmeyer NJ (2012) Predicting risk for venous thromboembolism with bariatric surgery. Ann Surg 255:1100–1104
Kearon C (2003) Natural history of venous thromboembolism. Circulation 107:22I–30
Thereaux J, Lesuffleur T, Czernichow S, Basdevant A, Msika S, Nocca D, Millat B, Fagot-Campagna A (2018) To what extent does posthospital discharge chemoprophylaxis prevent venous thromboembolism after bariatric surgery? Ann Surg 267:727–733
Hamad GG, Choban PS (2005) Enoxaparin for thromboprophylaxis in morbidly obese patients undergoing bariatric surgery: findings of the prophylaxis against VTE outcomes in bariatric surgery patients receiving enoxaparin (PROBE) study. Obes Surg 15:1368–1374
Aminian A, Andalib A, Khorgami Z, Cetin D, Burguera B, Bartholomew J, Schaur PR (2017) Who should get extended thromboprophylaxis after bariatric surgery? Ann Surg 265:143–150
American Society for Metabolic and Bariatric Surgery Clinical Issues Committee (2013) ASMBS updated position statement on prophylactic measures to reduce the risk of venous thromboembolism in bariatric surgery patients. Surg Obes Relat Dis 9:493–497
Barba CA, Harrington C, Loewen M (2009) Status of venous thromboembolism prophylaxis among bariatric surgeons: have we changed our practice during the past decade? Surg Obes Relat Dis 5:352–356
Ojo P, Asiyanbola B, Valin E, Reinhold R (2008) Post discharge prophylactic anticoagulation in gastric bypass patient-how safe? Obes Surg 18:791–796
Rasmussen MS, Jorgensen LN, Wille-Jørgensen P, Nielsen JD, Horn A, Mohn AC, Somod L, Olsen B (2006) Prolonged prophylaxis with dalteparin to prevent late thromboembolic complications in patients undergoing major abdominal surgery: a multicenter randomized open-label study. J Thromb Haemost 4:2384–2390
Felder S, Rasmussen MS, King R, Sklow B, Kwaan M, Madoff R, Jensen C (2019) Prolonged thromboprophylaxis with low molecular weight heparin for abdominal or pelvic surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004318.pub4,June8
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2008) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349
Caprini JA (2010) Risk assessment as a guide for the prevention of the many faces of venous thromboembolism. Am J Surg 199:S3–10
Cassidy MR, Rosenkranz P, McAneny D (2014) Reducing postoperative venous thromboembolism complications with a standardized risk-stratified prophylaxis protocol and mobilization program. J Am Coll Surg 218:1095–1104
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel JM, Sundararajan V (2011) Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173:676–682
Garrido MM, Kelley AS, Paris J, Roza K, Meier DE, Morrison RS, Aldridge MD (2014) Methods for constructing and assessing propensity scores. Health Serv Res 49:1701–1720
Zhehui Luo Z, Gardiner JC, Bradley CJ (2010) Applying propensity score methods in medical research: pitfalls and prospects. Med Care Res Rev 67:528–554
Austin PC (2009) The relative ability of different propensity score methods to balance measured covariates between treated and untreated subjects in observational studies. Med Decis Mak 29:661–677
Moulin P-A, Dutour A, Ancel P, Morange P-E, Bege T, Ziegler O, Berdah S, Frere C, Gaborit B (2017) Perioperative thromboprophylaxis in severely obese patients undergoing bariatric surgery: insights from a French national survey. Surg Obes Relat Dis 13:320–326
National Institute for Health and Care Excellence U (NICE; 2008). Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism|Guidance|NICE. https://www.nice.org.uk/guidance/ng89/chapter/Recommendations#Bariatricsurgery, May 30, 2020.
Samama C-M, Gafsou B, Jeandel T, Laporte S, Steib A, Marret E (2011) Prévention de la maladie thromboembolique veineuse postopératoire. Ann Fr Anesth Reanim 2011(30):947–951
Magee CJ, Barry J, Javed S, Macadam R, Kerrigan D (2010) Extended thromboprophylaxis reduces incidence of postoperative venous thromboembolism in laparoscopic bariatric surgery. Surg Obes Relat Dis 6:322–325
Pannucci CJ, Swistun L, MacDonald JK, Henke PK, Brooke BS (2017) Individualized venous thromboembolism risk stratification using the 2005 caprini score to identify the benefits and harms of chemoprophylaxis in surgical patients. Ann Surg 265:1094–1103
Caprini JA (2005) Thrombosis risk assessment as a guide to quality patient care. Dis Mon 51:70–78
Pannucci CJ, Bailey SH, Dreszer G, Fisher Wachtman C, Zumsteg JW, Jaber RM, Hamill JB, Hume KM, Rubin JP, Neligan PC, Kalliainen LK, Hoxworth RE, Pusic AL, Wilkins EG (2011) Validation of the Caprini risk assessment model in plastic and reconstructive surgery patients. J Am Coll Surg 212:105–112
Acknowledgements
Dr. Fennern is supported by a training grant from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number T32DK070555. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Erin B. Fennern, Farhood Farjah, Judy Y. Chen, Francys C. Verdial, Sara B. Cook, Erika M. Wolff, and Saurabh Khandelwal have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fennern, E.B., Farjah, F., Chen, J.Y. et al. Use of post-discharge heparin prophylaxis and the risk of venous thromboembolism and bleeding following bariatric surgery. Surg Endosc 35, 5531–5537 (2021). https://doi.org/10.1007/s00464-020-08049-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08049-7