Abstract
Background
The feasibility of laparoscopic surgery for primary appendiceal tumors compared to that of open surgery has not been demonstrated to date because primary appendiceal tumors are rare. This study aimed to compare the long-term outcomes between laparoscopic and open surgeries for primary appendiceal tumors.
Methods
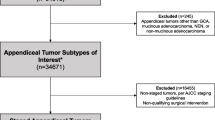
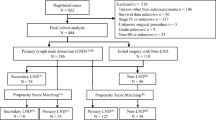
In this multicenter retrospective cohort study, the data of patients who had been histologically diagnosed with primary appendiceal tumors at 43 tertiary hospitals in Japan between 2000 and 2017 were analyzed. In total, 922 patients were assessed, and 679 cases were eligible for analysis. Using propensity scores, the baseline characteristics were matched for 114 open surgery cases and 114 laparoscopic surgery cases. The primary endpoints were recurrence-free survival (excluding patients with stage IV disease with distant metastasis) and overall survival.
Results
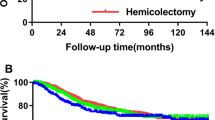
The rate of conversion from laparoscopic to open surgery was 1.5%. The 5-year recurrence-free survival rates were 80.4% (95% confidence interval: 71.0–89.7) and 78.2% (95% confidence interval: 69.0–87.3) in the laparoscopic and open surgery groups, respectively, with no significant difference (p = 0.57). No significant difference was observed in the 5-year overall survival rates between the laparoscopic [83.5% (95% confidence interval: 74.4–92.7)] and open surgery [72.7% (95% confidence interval: 62.3–83.0); p = 0.09] groups. In multivariate analysis, laparoscopic surgery was not identified as an independent prognostic factor for overall survival [hazard ratio: 0.49 (95% confidence interval: 0.23–1.06), p = 0.0707].
Conclusions
Laparoscopic surgery is comparable to open surgery and can be considered a treatment option for primary appendiceal tumors.


Similar content being viewed by others
Data availability
Dr. Inoue has full access to all data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
Connor SJ, Hanna GB, Frizelle FA (1998) Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7970 appendectomies. Dis Colon Rectum 41:75–80
Board WCoTE (2019) WHO classification of tumours: digestive system tumours, 5th edn. International Agency for Research on Cancer, Lyon, pp 135–152
Nelson H, Sargent DJ, Wieand HS et al (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Buunen M, Veldkamp R, Hop WC et al (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Bonjer HJ, Deijen CL, Abis GA et al (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
Ang CS-P, Shen JP, Hardy-Abeloos CJ et al (2018) Genomic landscape of appendiceal neoplasms. JCO Precis Oncol 2:1–18
Shaib WL, Assi R, Shamseddine A et al (2017) Appendiceal mucinous neoplasms: diagnosis and management. Oncologist 22:1107–1116
Sueda T, Murata K, Takeda T et al (2019) Survival outcomes of appendiceal mucinous neoplasms by histological type and stage: Analysis of 266 cases in a multicenter collaborative retrospective clinical study. Ann Gastroenterol Surg 3:291–300
Bucher P, Mathe Z, Demirag A et al (2004) Appendix tumors in the era of laparoscopic appendectomy. Surg Endosc 18:1063–1066
Bucher P, Gervaz P, Ris F et al (2006) Laparoscopic versus open resection for appendix carcinoid. Surg Endosc 20:967–970
Kim TK, Park JH, Kim JY et al (2018) Safety and feasibility of laparoscopic surgery for appendiceal mucocele: a multicenter study. Surg Endosc 32:4408–4414
Park KJ, Choi HJ, Kim SH (2015) Laparoscopic approach to mucocele of appendiceal mucinous cystadenoma: feasibility and short-term outcomes in 24 consecutive cases. Surg Endosc 29:3179–3183
James D, Brierley MKG, Wittekind C (2016) TNM classification of malignant tumours, 8th edn. Wiley-Blackwell, Hoboken, pp 70–72
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46:399–424
Rosenbaum PR, Rubin DB (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Lee WS, Choi ST, Lee JN et al (2011) A retrospective clinicopathological analysis of appendiceal tumors from 3,744 appendectomies: a single-institution study. Int J Colorectal Dis 26:617–621
Benedix F, Reimer A, Gastinger I et al (2010) Primary appendiceal carcinoma–epidemiology, surgery and survival: results of a German multi-center study. Eur J Surg Oncol 36:763–771
McCusker ME, Cote TR, Clegg LX et al (2002) Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973–1998. Cancer 94:3307–3312
Turaga KK, Pappas SG, Gamblin T (2012) Importance of histologic subtype in the staging of appendiceal tumors. Ann Surg Oncol 19:1379–1385
Overman MJ, Fournier K, Hu CY et al (2013) Improving the AJCC/TNM staging for adenocarcinomas of the appendix: the prognostic impact of histological grade. Ann Surg 257:1072–1078
Gonzalez-Moreno S, Sugarbaker PH (2004) Right hemicolectomy does not confer a survival advantage in patients with mucinous carcinoma of the appendix and peritoneal seeding. Br J Surg 91:304–311
Gonzalez-Moreno S, Brun E, Sugarbaker PH (2005) Lymph node metastasis in epithelial malignancies of the appendix with peritoneal dissemination does not reduce survival in patients treated by cytoreductive surgery and perioperative intraperitoneal chemotherapy. Ann Surg Oncol 12:72–80
Shabanzadeh DM, Sorensen LT (2012) Laparoscopic surgery compared with open surgery decreases surgical site infection in obese patients: a systematic review and meta-analysis. Ann Surg 256:934–945
Matsuda C, Ikenaga M (2018) Is surgical treatment necessary for uncomplicated acute appendicitis? Ann Gastroenterol Surg 2:394
Acknowledgments
We thank the following doctors for their cooperation during this study: M. Ikeda (Hyogo College of Medicine), M. Itabashi (Tokyo Women’s Medical University), Y. Ide (Yao Municipal Hospital), A. Iwashita (Fukuoka University Chikushi Hospital), Y. Ohno (Osaka University), S. Okamura (Suita Municipal Hospital), E. Oki (Kyushu University), H. Ozawa (Tochigi Cancer Center), T. Kato (Osaka National Hospital), M. Kishimoto (Kyoto Prefectural University of Medicine), K. Sakamoto (Juntendo University), A. Shiomi (Shizuoka Cancer Center Hospital), R. Shinkai (Saiseikai Senri Hospital), T. Sudo (Yamagata Prefectural Central Hospital), Y. Takii (Niigata Cancer Center Hospital), I. Takemasa (Sapporo Medical University), Y. Doki (Osaka University), M. Nakanishi (Kyoto Prefectural University of Medicine), S. Noura (Osaka Rosai Hospital), Y. Fukunaga (Cancer Institute Hospital), T. Furuhata (St. Marianna Medical University Toyoko Hospital), T. Mizushima (Osaka University), T. Yao (Juntendo University), K. Yamazaki (Shizuoka Cancer Center Hospital), H. Yokomizo (Tokyo Women’s Medical University Medical Center East), K. Yoshimatsu (Saiseikai Kurihashi Hospital), H. Takeyama (Minoh City Hospital), M. Tsujie (Sakai City Medical Center), H. Ohta (Ikeda City Hospital), M. Ikenaga (Higashiosaka City Medical Center), H. Mizuno (Nippon Life Hospital), A. Ogawa (Tane General Hospital), K. Yasumasa (Japan Community Healthcare Organization Osaka Hospital), K. Tamagawa (Otemae Hospital), H. Takemoto (Kinki Central Hospital), and M. Fukunaga (Hyogo Prefectural Nishinomiya Hospital).
Funding
There are no sources of funding to disclose.
Author information
Authors and Affiliations
Consortia
Contributions
AI—concept and design, Acquisition, analysis, or interpretation of data, Drafting of the manuscript, Statistical analysis. KM—Concept and design, Acquisition, analysis, or interpretation of data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content, Statistical analysis. TK—Concept and design, Acquisition, analysis, or interpretation of data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content. TT—Concept and design, Acquisition, analysis, or interpretation of data, Drafting of the manuscript, Statistical analysis. MF concept and design, Acquisition, analysis, or interpretation of data, Drafting of the manuscript, Statistical analysis. TY—Concept and design. TY—Concept and design. TM—Concept and design, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content. TS—Concept and design. SM—Concept and design. YS— Concept and design. MI— Concept and design. YK— Concept and design. MS— concept and design, Acquisition, analysis, or interpretation of data. MY— concept and design, Acquisition, analysis, or interpretation of data. YK— Concept and design, Acquisition, analysis, or interpretation of data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content. KS— Concept and design, Acquisition, analysis, or interpretation of data, Drafting of the manuscript, Critical revision of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Disclosures
Akira Inoue, Kohei Murata, Takamichi Komori, Takashi Takeda, Makoto Fujii, Tomohiro Yamaguchi, Tatsuro Yamaguchi, Toshiki Masuishi, Tetsuya Shiota, Shunji Morita, Yozo Suzuki, Masaaki Ito, Yukihide Kanemitsu, Manabu Shiozawa, Masayoshi Yasui, Yoshinori Kagawa, and Kenichi Sugihara have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Inoue, A., Murata, K., Komori, T. et al. Open versus laparoscopic surgery for primary appendiceal tumors: a large multicenter retrospective propensity score-matched cohort study in Japan. Surg Endosc 35, 5515–5523 (2021). https://doi.org/10.1007/s00464-020-08046-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08046-w