Abstract
Background
Utilization of minimally invasive surgery (MIS) has multiple determinants, one being the specialization of the surgeon. The purpose of this study was to assess the differences in the utilization of MIS, associated length of stay (LOS), and complications for colorectal cancer between colorectal (CRS) and general surgeons (GS). Previous studies have documented the influence of surgical volume and surgeon specialty on clinical outcomes and patient survival following colorectal cancer surgery. It is unclear whether there are differences in the utilization of MIS for colorectal cancer based on surgeon’s specialization and how this influences clinical outcomes.
Methods
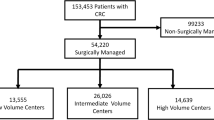
Using the 2013–2015 Florida Inpatient Discharge Dataset and the National Plan & Provider Enumeration System, colorectal cancer patients experiencing a colorectal surgery were identified as well as the operating physician’s specialty. Mixed-effects regression models were used to identify associations between the use of MIS, complications during the hospital stay, and patient LOS with patient, physician, and hospital characteristics.
Results
There is no difference in the use of MIS, complication, nor LOS between GS and CRS for colorectal cancer surgery. However, physician volume was associated with increased use of MIS (OR 1.26, 95% CI 1.09, 1.46) and MIS was associated with decreases in certain complications as well as reductions in LOS overall (β = − 0.16, p < 0.001) and for each specialty (GS: β = − 0.18, p < 0.001; CRS β = − 0.12, p < 0.001)
Conclusions
Despite the higher amount of proctectomies performed by CRS, no difference in MIS utilization, complication rate, or LOS was found for colorectal cancer patients based on surgeon specialty. While there are some differences in clinical outcomes attributable to specialized training, results from this study indicate that differences in surgical approach (MIS vs. Open), as well as the patient populations encountered by these two specialties, are key factors in the outcomes observed.
Similar content being viewed by others
References
Abu Gazala M, Wexner SD (2017) Re-appraisal and consideration of minimally invasive surgery in colorectal cancer. Gastroenterol Rep 5(1):1–10
Guend H, Lee DY, Myers EA, Gandhi ND, Cekic V, Whelan RL (2015) Technique of last resort: characteristics of patients undergoing open surgery in the laparoscopic era. Surg Endosc 29(9):2763–2769
Hollis RH, Cannon JA, Singletary BA, Korb ML, Hawn MT, Heslin MJ (2016) Understanding the value of both laparoscopic and robotic approaches compared to the open approach in colorectal surgery. J Laparoendosc Adv Surg Tech Part A 26(11):850–856
Moghadamyeghaneh Z, Hanna MH, Carmichael JC, Pigazzi A, Stamos MJ, Mills S (2016) Comparison of open, laparoscopic, and robotic approaches for total abdominal colectomy. Surg Endosc 30(7):2792–2798
Dorrance HR, Docherty GM, O’Dwyer PJ (2000) Effect of surgeon specialty interest on patient outcome after potentially curative colorectal cancer surgery. Dis Colon Rectum 43(4):492–498
Read TE, Myerson RJ, Fleshman JW et al (2002) Surgeon specialty is associated with outcome in rectal cancer treatment. Dis Colon Rectum 45(7):904–914
McArdle CS, Hole DJ (2004) Influence of volume and specialization on survival following surgery for colorectal cancer. Br J Surg 91(5):610–617
CCS H. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. Available at https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Published 2017. Updated March 6, 2017. Accessed 14 Nov 2018
System NPPE. NPPES NPI Registry. Available at https://npiregistry.cms.hhs.gov. Published 2019. Accessed 15 Aug 2019
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36(1):8–27
Health FDo. Rural County List. Available at https://www.floridahealth.gov/programs-and-services/community-health/rural-health/_documents/rual-counties-2000-2010.pdf. Published 2018. Accessed 2018
Yamamoto T, Keighley MR (1999) Proctocolectomy is associated with a higher complication rate but carries a lower recurrence rate than total colectomy and ileorectal anastomosis in Crohn colitis. Scand J Gastroenterol 34(12):1212–1215
Saraidaridis JT, Hashimoto DA, Chang DC, Bordeianou LG, Kunitake H (2018) Colorectal surgery fellowship improves in-hospital mortality after colectomy and proctectomy irrespective of hospital and surgeon volume. J Gastrointest Surg Off J Soc Surg Aliment Tract 22(3):516–522
Hodgson DC, Fuchs CS, Ayanian JZ (2001) Impact of patient and provider characteristics on the treatment and outcomes of colorectal cancer. J Natl Cancer Inst 93(7):501–515
Salz T, Sandler RS (2008) The effect of hospital and surgeon volume on outcomes for rectal cancer surgery. Clin Gastroenterol Hepatol 6(11):1185–1193
Osagiede O, Spaulding AC, Cochuyt JJ et al (2018) Disparities in minimally invasive surgery for colorectal cancer in Florida. Am J Surg. 218:293–301
Mehta A, Xu T, Hutfless S et al (2017) patient, surgeon, and hospital disparities associated with benign hysterectomy approach and perioperative complications. Am J Obstet Gynecol 216(5):497e491–497 e410
Tamirisa NP, Sheffield KM, Parmar AD et al (2015) Surgeon and facility variation in the use of minimally invasive breast biopsy in Texas. Ann Surg 262(1):171–178
Eisenkop SM, Spirtos NM, Montag TW, Nalick RH, Wang HJ (1992) The impact of subspecialty training on the management of advanced ovarian cancer. Gynecol Oncol 47(2):203–209
Kehoe S, Powell J, Wilson S, Woodman C (1994) The influence of the operating surgeon’s specialisation on patient survival in ovarian carcinoma. Br J Cancer 70(5):1014–1017
Funding
This work was supported by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Drs. Osagiede, Haehn, Spaulding, Otto, Cochuyt, Lemini, Merchea, Kelly, and Colibaseanu have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Osagiede, O., Haehn, D.A., Spaulding, A.C. et al. Influence of surgeon specialty and volume on the utilization of minimally invasive surgery and outcomes for colorectal cancer: a retrospective review. Surg Endosc 35, 5480–5488 (2021). https://doi.org/10.1007/s00464-020-08039-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08039-9