Abstract
Introduction
In complex abdominal wall reconstruction (AWR), the role of concomitant panniculectomy has been debated due to concern for increased wound complications that impact outcomes; however, long-term outcomes and quality of life (QOL) have not been well described. The aim of our study was to evaluate the outcomes and QOL in patients undergoing AWR with panniculectomy utilizing 3D volumetric-based propensity match.
Methods
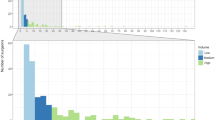
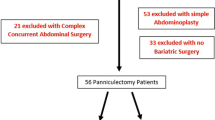
A prospective database from a tertiary referral hernia center was queried for patients undergoing open AWR. 3D CT volumetrics were analyzed and a propensity match comparing AWR patients with and without panniculectomy was created including subcutaneous fat volume (SFV). QOL was analyzed using the Carolinas Comfort Scale.
Results
Propensity match yielded 312 pairs, all with adequate CT imaging for volumetric analysis. The panniculectomy group had a higher BMI (p = 0.03) and were more likely female (p < 0.0001), but all other demographics and comorbidities were similar. The panniculectomy group was more likely to have undergone prior hernia repair (77% vs 64%, p < 0.001), but hernia area, SFV, and CDC wound class were similar (all p > 0.05). Requirement of component separation (61% vs 50%, p = 0.01) and mesh excision (44% vs 35%, p = 0.02) were higher in the panniculectomy group, but operative time were similar (all p ≥ 0.05). Panniculectomy patients had a higher overall wound occurrence rate (45% vs 32%, p = 0.002) which was differentiated only by a higher rate of wound breakdown (24% vs 14%, p = 0.003); all other specific wound complications were equal (all p ≥ 0.05). Hernia recurrence rates were similar (8% vs 9%, p = 0.65) with an average follow-up of 28 months. Overall QOL was equal at 2 weeks, and 1, 6, and 12 months (all p ≥ 0.05).
Conclusions
Despite panniculectomy patients and their hernias being more complex, concomitant panniculectomy increased wound complications but did not negatively impact infection rates or long-term outcomes. Concomitant panniculectomy should be considered in appropriate patients to avoid two procedures.

Similar content being viewed by others
References
Fischer JP, Basta MN, Wink JD, Wes AM, Kovach SJ (2014) Optimizing patient selection in ventral hernia repair with concurrent panniculectomy: an analysis of 1974 patients from the ACS-NSQIP datasets. J Plast Reconstr Aesthet Surg 67:1532–1540. https://doi.org/10.1016/j.bjps.2014.07.001
Giordano SA, Garvey PB, Baumann DP, Liu J, Butler CE (2017) The impact of body mass index on abdominal wall reconstruction outcomes: a comparative study. Plast Reconstr Surg 139:1234–1244. https://doi.org/10.1097/PRS.0000000000003264
Koolen PGL, Ibrahim AMS, Kim K, Sinno HH, Lee BT, Schneider BE, Jones DB, Lin SJ (2014) Patient selection optimization following combined abdominal procedures: analysis of 4925 patients undergoing Panniculectomy/Abdominoplasty with or without concurrent hernia repair. Plast Reconstr Surg 134:539e–550e. https://doi.org/10.1097/PRS.0000000000000519
Centers for Disease Control and Prevention (2010) Vital signs: state-specific obesity prevalence among adults - United States, 2009. Morb Mortal Wkly Rep 59:951–955
Petty P, Manson PN, Black R, Romano JJ, Sitzman J, Vogel J (1992) Panniculus morbidus. Ann Plast Surg 28:442–452. https://doi.org/10.1097/00000637-199205000-00008
Chiswick C, Cooper ES, Norman JE, Denison FC (2012) Fat necrosis of the abdominal pannus following caesarean section in patients with morbid obesity. Eur J Obstet Gynecol Reprod Biol 160:118–119. https://doi.org/10.1016/j.ejogrb.2011.09.045
Giordano S, Garvey PB, Baumann DP, Liu J, Butler CE (2017) Concomitant panniculectomy affects wound morbidity but not hernia recurrence rates in abdominal wall reconstruction: a propensity score analysis. Plast Reconstr Surg 140:1263–1273. https://doi.org/10.1097/PRS.0000000000003855
Ross SW, Wormer BA, Kim M, Oommen B, Bradley JF, Lincourt AE, Augenstein VA, Heniford BT (2015) Defining surgical outcomes and quality of life in massive ventral hernia repair: an international multicenter prospective study. Am J Surg 210:801–813. https://doi.org/10.1016/j.amjsurg.2015.06.020
Berry MF, Paisley S, Low DW, Rosato EF (2007) Repair of large complex recurrent incisional hernias with retromuscular mesh and panniculectomy. Am J Surg 194:199–204. https://doi.org/10.1016/j.amjsurg.2006.10.031
Espinosa-de-Los-Monteros A, Avendaño-Peza H, Gómez-Arcive Z, Martin-Del-Campo LA, Navarro-Navarro J-A (2016) Total abdominal wall reconstruction with component separation, reinforcement, and vertical abdominoplasty in patients with complex ventral hernias. Aesthet Plast Surg 40:387–394. https://doi.org/10.1007/s00266-016-0628-7
Fischer JP, Wink JD, Tuggle CT, Nelson JA, Kovach SJ (2015) Wound risk assessment in ventral hernia repair: generation and internal validation of a risk stratification system using the ACS-NSQIP. Hernia 19:103–111. https://doi.org/10.1007/s10029-014-1318-5
McNichols CHL, Diaconu S, Liang Y, Ikheloa E, Kumar S, Kumar S, Nam A, Rasko Y (2018) Outcomes of ventral hernia repair with concomitant panniculectomy. Ann Plast Surg 80:391–394. https://doi.org/10.1097/SAP.0000000000001277
Shubinets V, Fox JP, Tecce MG, Mirzabeigi MN, Lanni MA, Kelz RR, Dumon KR, Kovach SJ, Fischer JP (2017) Concurrent panniculectomy in the obese ventral hernia patient: assessment of short-term complications, hernia recurrence, and healthcare utilization. J Plast Reconstr Aesthet Surg 70:759–767. https://doi.org/10.1016/j.bjps.2017.01.001
Warren JA, Epps M, Debrux C, Fowler JL, Ewing JA, Cobb WS, Carbonell AM (2015) Surgical site occurrences of simultaneous panniculectomy and incisional hernia repair. Am Surg 81:764–769
Zemlyak AY, Colavita PD, El Djouzi S, Walters AL, Hammond L, Hammond B, Tsirline VB, Getz S, Heniford BT (2012) Comparative study of wound complications: isolated panniculectomy versus panniculectomy combined with ventral hernia repair. J Surg Res 177:387–391. https://doi.org/10.1016/j.jss.2012.06.029
Kao AM, Ross SW, Otero J, Maloney SR, Prasad T, Augenstein VA, Heniford BT, Colavita PD (2019) Use of computed tomography volumetric measurements to predict operative techniques in paraesophageal hernia repair. Surg Endosc. https://doi.org/10.1007/s00464-019-06930-8
Schlosser KA, Maloney SR, Prasad T, Colavita PD, Augenstein VA, Heniford BT (2019) Three-dimensional hernia analysis: the impact of size on surgical outcomes. Surg Endosc. https://doi.org/10.1007/s00464-019-06931-7
Schlosser KA, Maloney SR, Prasad T, Colavita PD, Augenstein VA, Heniford BT (2019) Too big to breathe: predictors of respiratory failure and insufficiency after open ventral hernia repair. Surg Endosc. https://doi.org/10.1007/s00464-019-07181-3
Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, Sing RF, Augenstein VA (2018) Carolinas comfort scale as a measure of hernia repair quality of life. Ann Surg 267:171–176. https://doi.org/10.1097/SLA.0000000000002027
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg 206:638–644. https://doi.org/10.1016/j.jamcollsurg.2007.11.025
Hutchison CE, Rhemtulla IA, Mauch JT, Broach RB, Enriquez FA, Hernandez JA, Messa CA, Williams NN, Harbison SP, Fischer JP (2019) Cutting through the fat: a retrospective analysis of clinical outcomes, cost, and quality of life with the addition of panniculectomy to ventral hernia repair in overweight patients. Hernia 23:969–977. https://doi.org/10.1007/s10029-019-02024-5
Maloney SR, Schlosser KA, Prasad T, Kasten KR, Gersin KS, Colavita PD, Kercher KW, Augenstein VA, Heniford BT (2019) Twelve years of component separation technique in abdominal wall reconstruction. Surg (United States) 166:435–444. https://doi.org/10.1016/j.surg.2019.05.043
Jolissaint JS, Dieffenbach BV, Tsai TC, Pernar LI, Shoji BT, Ashley SW, Tavakkoli A (2020) Surgical site occurrences, not body mass index, increase the long-term risk of ventral hernia recurrence. Surgery (United States). Mosby Inc., St. Louis, pp 765–771
Heniford BT, Ross SW, Wormer BA, Walters AL, Lincourt AE, Colavita PD, Kercher KW, Augenstein VA (2020) Preperitoneal ventral hernia repair: a decade long prospective observational study with analysis of 1023 patient outcomes. Ann Surg 271:364–374. https://doi.org/10.1097/SLA.0000000000002966
Novitsky YW, Orenstein SB (2013) Effect of patient and hospital characteristics on outcomes of elective ventral hernia repair in the United States. Hernia 17:639–645. https://doi.org/10.1007/s10029-013-1088-5
Manilich E, Vogel JD, Kiran RP, Church JM, Seyidova-Khoshknabi D, Remzi FH (2013) Key factors associated with postoperative complications in patients undergoing colorectal surgery. Dis Colon Rectum 56:64–71. https://doi.org/10.1097/DCR.0b013e31827175f6
Di Martino M, Nahas FX, Kimura AK, Sallum N, Ferreira LM (2015) Natural evolution of seroma in abdominoplasty. Plast Reconstr Surg 135:691e–698e. https://doi.org/10.1097/PRS.0000000000001122
Gutowski KA (2018) Evidence-based medicine: abdominoplasty. Plast Reconstr Surg 141:286E–299E. https://doi.org/10.1097/PRS.0000000000004232
Huntington C, Jachthuber CE, Cox TC, Blair LJ, Getz SB, Augenstein VA, Heniford BT (2015) Panniculectomy with open ventral hernia repair: a prospective, randomized (by Insurance) study. J Am Coll Surg 221:S117–S118. https://doi.org/10.1016/j.jamcollsurg.2015.07.275
Bhayani NH, Hyder O, Frederick W, Schulick RD, Wolgang CL, Hirose K, Edil B, Herman JM, Choti MA, Pawlik TM (2012) Effect of metabolic syndrome on perioperative outcomes after liver surgery: a National Surgical Quality Improvement Program (NSQIP) analysis. Surgery 152:218–226. https://doi.org/10.1016/j.surg.2012.05.037
Glance LG, Wissler R, Mukamel DB, Li Y, Diachun CAB, Salloum R, Fleming FJ, Dick AW (2010) Perioperative outcomes among patients with the modified metabolic syndrome who are undergoing noncardiac surgery. Anesthesiology 113:859–872. https://doi.org/10.1097/ALN.0b013e3181eff32e
Papadopulos NA, Staffler V, Mirceva V, Henrich G, Papadopoulos ON, Kovacs L, Herschbach P, MacHens HG, Biemer E (2012) Does abdominoplasty have a positive influence on quality of life, self-esteem, and emotional stability? Plast Reconstr Surg 129:957e–962e
Papadopulos NA, Meier AC, Henrich G, Herschbach P, Kovacs L, Machens HG, Klöppel M (2019) Aesthetic abdominoplasty has a positive impact on quality of life prospectively. J Plast Reconstr Aesthet Surg 72:813–820. https://doi.org/10.1016/j.bjps.2018.12.020
Schlosser KA, Maloney SR, Gbozah K, Prasad T, Colavita PD, Augenstein VA, Heniford BT (2020) The impact of weight change on intra-abdominal and hernia volumes. Surg (United States). https://doi.org/10.1016/j.surg.2020.01.007
Rosen MJ, Aydogdu K, Grafmiller K, Petro CC, Faiman GH, Prabhu A (2015) A multidisciplinary approach to medical weight loss prior to complex abdominal wall reconstruction: is it feasible? J Gastrointest Surg 19:1399–1406. https://doi.org/10.1007/s11605-015-2856-6
Staalesen T, Olsen MF, Elander A (2015) The effect of abdominoplasty and outcome of rectus fascia plication on health-related quality of life in post-bariatric surgery patients. Plast Reconstr Surg 136:750e–761e. https://doi.org/10.1097/PRS.0000000000001772
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Augenstein has received honoraria for speaking for Medtronic, Allergan, Intuitive, Acelity, and W.L. Gore. Dr. Heniford has been awarded surgical education grants and honoraria from W.L. Gore and Allergan. Dr. Colavita is a consultant for design of a research protocol for Becton Dickinson. Dr. Kercher has received honoraria for speaking for Bard and Ethicon. Dr. Elhage, Dr. Marturano, Dr. Deerenberg, Dr. Shao, and Ms. Prasad have no potential conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elhage, S.A., Marturano, M.N., Deerenberg, E.B. et al. Impact of panniculectomy in complex abdominal wall reconstruction: a propensity matched analysis in 624 patients. Surg Endosc 35, 5287–5294 (2021). https://doi.org/10.1007/s00464-020-08011-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-08011-7