Abstract
Background
Laparoscopic Heller myotomy fails in approximately 3.5% to 15% of patients. Evidence of successful laparoscopic reoperation is limited to a few studies.
Methods
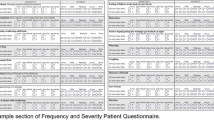
This case–control study was conducted in patients who underwent laparoscopic Heller myotomy reoperation (LHM-R) from 2008 to 2016. The operative outcomes, preoperative and last follow-up manometric parameters, and symptom questionnaire results, including the Eckardt, Gastroesophageal Reflux Disease-Health Related Quality of Life (GERD-HRQL) and eating assessment tool (EAT-10) scores, were obtained. The data were compared with those of patients who underwent primary laparoscopic Heller myotomy (LHM-1).
Results
Thirty-five patients who underwent LHM-R and 35 patients who underwent LHM-1 were included. The reasons for failure in the LHM-R patient group included incomplete myotomy (71.4%), myotomy fibrosis (25.7%) and structural alterations in fundoplication (2.9%). The follow-up duration was 34 months for the LHM-R group and 24 months for the LHM-1 group (p = 0.557). The procedure was performed by laparoscopy in 100% of the patients in the two groups. No differences were found regarding surgical morbidity (11.4% LHM-R vs. 2.9% LHM-1, p = 0.164). The symptomatic outcomes were equivalent between groups (Eckardt p = 0.063, EAT–10 p = 0.166, GERD–HRQL p = 0.075). An IRP < 15 mmHg was achieved in 100% of the LHM-R and LHM-1 patients. At the last follow-up, 82.1% of the LHM-R patients and 91.4% of the LHM-1 patients were in symptomatic remission (p = 0.271).
Conclusion
The results achieved with LHM-R are similar to those achieved with LHM-1. Laparoscopic reoperation should be considered an effective and safe treatment after a failed Heller myotomy.
Similar content being viewed by others
References
Furuzawa-Carballeda J, Aguilar-León D, Gamboa-Domínguez A, Valdovinos MA, Nuñez-Álvarez C, Martín-del-Campo LA, Enríquez AB, Coss-Adame E, Svarch AE, Flores-Nájera A, Villa-Baños A, Ceballos JC, Torres-Villalobos G (2015) Achalasia—An autoimmune inflammatory disease: a cross-sectional study. J Immunol Res 2015:1–18. https://doi.org/10.1155/2015/729217
Furuzawa-Carballeda J, Torres-Landa S, Valdovinos MÁ, Coss-Adame E, Martín-del-Campo LA, Torres-Villalobos G (2016) New insights into the pathophysiology of achalasia and implications for future treatment. World J Gastroenterol 22:7892–7907. https://doi.org/10.3748/wjg.v22.i35.7892
Furuzawa-Carballeda J, Zuñiga J, Hernández-Zaragoza DI, Barquera R, Marques-García E, Jiménez-Alvarez L, Cruz-Lagunas A, Ramírez G, Regino NE, Espinosa-Soto R, Yunis EJ, Romero-Hernández F, Azamar-Llamas D, Coss-Adame E, Valdovinos MA, Torres-Landa S, Palacios-Ramírez A, Breña B, Alejandro-Medrano E, Hernández-Ávila A, Granados J, Torres-Villalobos G (2018) An original Eurasian haplotype, HLA-DRB1*14:54-DQB1*05:03, influences the susceptibility to idiopathic achalasia. PLoS ONE 13:e0201676. https://doi.org/10.1371/journal.pone.0201676
Verne GN, Hahn AB, Pineau BC, Hoffman BJ, Wojciechowski BW, Wu WC (1999) Association of HLA-DR and -DQ alleles with idiopathic achalasia. Gastroenterology 117:26–31
Williams VA, Peters JH (2009) Achalasia of the esophagus: a surgical disease. J Am Coll Surg 208:151–162. https://doi.org/10.1016/j.jamcollsurg.2008.08.027
Schlottmann F, Luckett DJ, Fine J, Shaheen NJ, Patti MG (2018) Laparoscopic Heller myotomy versus peroral endoscopic myotomy (POEM) for achalasia: a systematic review and meta-analysis. Ann Surg 267:451–460. https://doi.org/10.1097/SLA.0000000000002311
Rossetti G, Brusciano L, Amato G, Maffettone V, Napolitano V, Russo G, Izzo D, Russo F, Pizza F, del Genio G, del Genio A (2005) A total fundoplication is not an obstacle to esophageal emptying after Heller myotomy for Achalasia. Ann Surg 241:614–621. https://doi.org/10.1097/01.sla.0000157271.69192.96
Jeansonne LO, White BC, Pilger KE, Shane MD, Zagorski S, Davis SS, Hunter JG, Lin E, Smith CD (2007) Ten-year follow-up of laparoscopic Heller myotomy for achalasia shows durability. Surg Endosc 21:1498–1502. https://doi.org/10.1007/s00464-007-9500-9
Ortiz A, de Haro LFM, Parrilla P, Lage A, Perez D, Munitiz V, Ruiz D, Molina J (2008) Very long-term objective evaluation of heller myotomy plus posterior partial fundoplication in patients with achalasia of the cardia. Ann Surg 247:258–264. https://doi.org/10.1097/SLA.0b013e318159d7dd
Cowgill SM, Villadolid D, Boyle R, Al-Saadi S, Ross S, Rosemurgy AS (2009) Laparoscopic Heller myotomy for achalasia: results after 10 years. Surg Endosc 23:2644–2649. https://doi.org/10.1007/s00464-009-0508-1
Costantini M, Salvador R, Capovilla G, Vallese L, Costantini A, Nicoletti L, Briscolini D, Valmasoni M, Merigliano S (2019) A thousand and one laparoscopic Heller myotomies for esophageal achalasia: a 25-year experience at a single tertiary center. J Gastrointest Surg 23:23–35. https://doi.org/10.1007/s11605-018-3956-x
Petersen RP, Pellegrini CA (2010) Revisional surgery after Heller myotomy for esophageal achalasia. Surg Laparosc Endosc Percutan Technol 20:321–325. https://doi.org/10.1097/SLE.0b013e3181f39fdb
Zaninotto G, Costantini M, Portale G, Battaglia G, Molena D, Carta A, Costantino M, Nicoletti L, Ancona E (2002) Etiology, diagnosis, and treatment of failures after laparoscopic Heller myotomy for achalasia. Ann Surg 235:186–192
Vela MF, Richter JE, Wachsberger D, Connor J, Rice TW (2004) Complexities of managing achalasia at a tertiary referral center: use of pneumatic dilatation, Heller myotomy, and botulinum toxin injection. Am J Gastroenterol 99:1029–1036. https://doi.org/10.1111/j.1572-0241.2004.30199.x
Guardino JM, Vela MF, Connor JT, Richter JE (2004) Pneumatic dilation for the treatment of achalasia in untreated patients and patients with failed Heller myotomy. J Clin Gastroenterol 38:855–860
Chen Z, Bessell JR, Chew A, Watson DI (2010) Laparoscopic cardiomyotomy for achalasia: clinical outcomes beyond 5 years. J Gastrointest Surg 14:594–600. https://doi.org/10.1007/s11605-010-1158-2
Kumbhari V, Behary J, Szczesniak M, Zhang T, Cook IJ (2013) Efficacy and safety of pneumatic dilatation for achalasia in the treatment of post-myotomy symptom relapse. Am J Gastroenterol 108:1076–1081. https://doi.org/10.1038/ajg.2013.32
Legros L, Ropert A, Brochard C, Bouguen G, Pagenault M, Siproudhis L, Bretagne J-F (2014) Long-term results of pneumatic dilatation for relapsing symptoms of achalasia after Heller myotomy. Neurogastroenterol Motil 26:1248–1255. https://doi.org/10.1111/nmo.12380
Saleh CMG, Ponds FAM, Schijven MP, Smout AJPM, Bredenoord AJ (2016) Efficacy of pneumodilation in achalasia after failed Heller myotomy. Neurogastroenterol Motil 28:1741–1746. https://doi.org/10.1111/nmo.12875
Amani M, Fazlollahi N, Shirani S, Malekzadeh R, Mikaeli J (2016) Assessment of pneumatic balloon dilation in patients with symptomatic relapse after failed Heller myotomy: a single center experience. Middle East J Dig Dis 8:57–62. https://doi.org/10.15171/mejdd.2016.08
Onimaru M, Inoue H, Ikeda H, Yoshida A, Santi EG, Sato H, Ito H, Maselli R, Kudo S-E (2013) Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: a single center prospective study. J Am Coll Surg 217:598–605. https://doi.org/10.1016/j.jamcollsurg.2013.05.025
Vigneswaran Y, Yetasook AK, Zhao J-C, Denham W, Linn JG, Ujiki MB (2014) Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg 18:1071–1076. https://doi.org/10.1007/s11605-014-2496-2
Ngamruengphong S, Inoue H, Ujiki MB, Patel LY, Bapaye A, Desai PN, Dorwat S, Nakamura J, Hata Y, Balassone V, Onimaru M, Ponchon T, Pioche M, Roman S, Rivory J, Mion F, Garros A, Draganov PV, Perbtani Y, Abbas A, Pannu D, Yang D, Perretta S, Romanelli J, Desilets D, Hayee B, Haji A, Hajiyeva G, Ismail A, Chen Y-I, Bukhari M, Haito-Chavez Y, Kumbhari V, Saxena P, Talbot M, Chiu PW-Y, Yip H-C, Wong VW-Y, Hernaez R, Maselli R, Repici A, Khashab MA (2017) Efficacy and safety of peroral endoscopic myotomy for treatment of achalasia after failed Heller myotomy. Clin Gastroenterol Hepatol 15:1531–1537.e3. https://doi.org/10.1016/j.cgh.2017.01.031
Howard JM, Ryan L, Lim KT, Reynolds JV (2011) Oesophagectomy in the management of end-stage achalasia - case reports and a review of the literature. Int J Surg 9:204–208. https://doi.org/10.1016/j.ijsu.2010.11.010
Veenstra BR, Goldberg RF, Bowers SP, Thomas M, Hinder RA, Smith CD (2016) Revisional surgery after failed esophagogastric myotomy for achalasia: successful esophageal preservation. Surg Endosc 30:1754–1761. https://doi.org/10.1007/s00464-015-4423-3
Loviscek MF, Wright AS, Hinojosa MW, Petersen R, Pajitnov D, Oelschlager BK, Pellegrini CA (2013) Recurrent dysphagia after Heller myotomy: is esophagectomy always the answer? J Am Coll Surg 216:736–743. https://doi.org/10.1016/j.jamcollsurg.2012.12.008 (discussion 743–4)
Grotenhuis BA, Wijnhoven BPL, Myers JC, Jamieson GG, Devitt PG, Watson DI (2007) Reoperation for dysphagia after cardiomyotomy for achalasia. Am J Surg 194:678–682. https://doi.org/10.1016/j.amjsurg.2007.01.035
Iqbal A, Tierney B, Haider M, Salinas VK, Karu A, Turaga KK, Mittal SK, Filipi CJ (2006) Laparoscopic re-operation for failed Heller myotomy. Dis Esophagus 19:193–199. https://doi.org/10.1111/j.1442-2050.2006.00564.x
Rosemurgy AS, Morton CA, Rosas M, Albrink M, Ross SB (2010) A single institution's experience with more than 500 laparoscopic Heller myotomies for achalasia. J Am Coll Surg 210:637–645. https://doi.org/10.1016/j.jamcollsurg.2010.01.035
Schuchert MJ, Luketich JD, Landreneau RJ, Kilic A, Gooding WE, Alvelo-Rivera M, Christie NA, Gilbert S, Pennathur A (2008) Minimally-invasive esophagomyotomy in 200 consecutive patients: factors influencing postoperative outcomes. Ann Thorac Surg 85:1729–1734. https://doi.org/10.1016/j.athoracsur.2007.11.017
Torquati A, Richards WO, Holzman MD, Sharp KW (2006) Laparoscopic myotomy for achalasia. Ann Surg 243:587–593. https://doi.org/10.1097/01.sla.0000216782.10502.47
Wright AS, Williams CW, Pellegrini CA, Oelschlager BK (2007) Long-term outcomes confirm the superior efficacy of extended Heller myotomy with Toupet fundoplication for achalasia. Surg Endosc 21:713–718. https://doi.org/10.1007/s00464-006-9165-9
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, Portale G, Nicoletti L, Cavallin F, Battaglia G, Ruol A, Ancona E (2008) Four hundred laparoscopic myotomies for esophageal achalasia: a single centre experience. Ann Surg 248:986–993. https://doi.org/10.1097/SLA.0b013e3181907bdd
Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, Fanelli RD, Society of American Gastrointestinal, and Endoscopic Surgeons (2012) SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc 26:296–311. https://doi.org/10.1007/s00464-011-2017-2
Yano F, Omura N, Tsuboi K, Hoshino M, Yamamoto S, Akimoto S, Masuda T, Kashiwagi H, Yanaga K (2017) Learning curve for laparoscopic Heller myotomy and Dor fundoplication for achalasia. PLoS ONE 12:e0180515. https://doi.org/10.1371/journal.pone.0180515
Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108:1238–1250. https://doi.org/10.1038/ajg.2013.196
Rossetti G, del Genio G, Maffettone V, Fei L, Brusciano L, Limongelli P, Pizza F, Tolone S, Di Martino M, del Genio F, del Genio A (2009) Laparoscopic reoperation with total fundoplication for failed Heller myotomy: is it a possible option? Personal experience and review of literature. Int Surg 94:330–334
Gockel I, Timm S, Sgourakis GG, Musholt TJ, Rink AD, Lang H (2010) Achalasia–if surgical treatment fails: analysis of remedial surgery. J Gastrointest Surg 14(Suppl 1):S46–57. https://doi.org/10.1007/s11605-009-1018-0
El Kafsi J, Foliaki A, Dehn TCB, Maynard ND (2016) Management of achalasia in the UK, do we need new guidelines? Ann Med Surg (Lond) 12:32–36. https://doi.org/10.1016/j.amsu.2016.10.009
Zaninotto G, Bennett C, Boeckxstaens G, Costantini M, Ferguson MK, Pandolfino JE, Patti MG, Ribeiro U, Richter J, Swanstrom L, Tack J, Triadafilopoulos G, Markar SR, Salvador R, Faccio L, Andreollo NA, Cecconello I, Costamagna G, da Rocha JRM, Hungness ES, Fisichella PM, Fuchs KH, Gockel I, Gurski R, Gyawali CP, Herbella FAM, Holloway RH, Hongo M, Jobe BA, Kahrilas PJ, Katzka DA, Dua KS, Liu D, Moonen A, Nasi A, Pasricha PJ, Penagini R, Perretta S, Sallum RAA, Sarnelli G, Savarino E, Schlottmann F, Sifrim D, Soper N, Tatum RP, Vaezi MF, van Herwaarden-Lindeboom M, Vanuytsel T, Vela MF, Watson DI, Zerbib F, Gittens S, Pontillo C, Vermigli S, Inama D, Low DE (2018) The 2018 ISDE achalasia guidelines. Dis Esophagus 31:83. https://doi.org/10.1093/dote/doy071
Bonatti H, Hinder RA, Klocker J, Neuhauser B, Klaus A, Achem SR, de Vault K (2005) Long-term results of laparoscopic Heller myotomy with partial fundoplication for the treatment of achalasia. Am J Surg 190:874–878. https://doi.org/10.1016/j.amjsurg.2005.08.012
Zaninotto G, Annese V, Costantini M, del Genio A, Costantino M, Epifani M, Gatto G, Donofrio V, Benini L, Contini S, Molena D, Battaglia G, Tardio B, Andriulli A, Ancona E (2004) Randomized controlled trial of botulinum toxin versus laparoscopic Heller myotomy for esophageal achalasia. Ann Surg 239:364–370. https://doi.org/10.1097/01.sla.0000114217.52941.c5
Oelschlager BK, Chang L, Pellegrini CA (2003) Improved outcome after extended gastric myotomy for achalasia. Arch Surg 138:490–495. https://doi.org/10.1001/archsurg.138.5.490 (discussion 495–7)
Csendes A, Braghetto I, Henriquez A, Cortes C (1989) Late results of a prospective randomised study comparing forceful dilatation and oesophagomyotomy in patients with achalasia. Gut 30:299–304. https://doi.org/10.1136/gut.30.3.299
Bonavina L, Nosadini A, Bardini R, Baessato M, Peracchia A (1992) Primary treatment of esophageal achalasia. Long-term results of myotomy and Dor fundoplication. Arch Surg 127:222–226 (discussion 227)
Torres-Villalobos G, Coss-Adame E, Furuzawa-Carballeda J, Romero-Hernández F, Blancas-Breña B, Torres-Landa S, Palacios-Ramírez A, Alejandro-Medrano E, Hernández-Ávila A, Flores-Najera A, Ávila Escobedo LM, Ramírez Angulo C, Rodríguez-Garcés A, Valdovinos MÁ (2017) Dor vs toupet fundoplication after laparoscopic Heller myotomy: long-term randomized controlled trial evaluated by high-resolution manometry. J Gastrointest Surg 108:1238–1310. https://doi.org/10.1007/s11605-017-3578-8
Bove A, Corbellini L, Catania A, Chiarini S, Bongarzoni G, Stella S, De Antoni E, De Matteo G (2001) Surgical controversies in the treatment of recurrent achalasia of the esophagus. Hepatogastroenterology 48:715–717
Gorecki PJ, Hinder RA, Libbey JS, Bammer T, Floch N (2002) Redo laparoscopic surgery for achalasia. Surg Endosc 16:772–776. https://doi.org/10.1007/s00464-001-8178-7
Duffy PE, Awad ZT, Filipi CJ (2003) The laparoscopic reoperation of failed Heller myotomy. Surg Endosc 17:1046–1049. https://doi.org/10.1007/s00464-002-8570-y
Rakita S, Villadolid D, Kalipersad C, Thometz D, Rosemurgy A (2007) Outcomes promote reoperative Heller myotomy for symptoms of achalasia. Surg Endosc 21:1709–1714. https://doi.org/10.1007/s00464-007-9226-8
Zeidan A, Ramez Salem M, Bamadhaj M, Maherzi A (2017) Is cricoid pressure effective in patients with achalasia? J Clin Anesth 38:117–118. https://doi.org/10.1016/j.jclinane.2017.01.039
Rice MJ, Mancuso AA, Gibbs C, Morey TE, Gravenstein N, Deitte LA (2009) Cricoid pressure results in compression of the postcricoid hypopharynx: the esophageal position is irrelevant. Anesth Analg 109:1546–1552. https://doi.org/10.1213/ane.0b013e3181b05404
Smith KJ, Dobranowski J, Yip G, Dauphin A, Choi PT-L (2003) Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anesthesiology 99:60–64
Zeidan AM, Salem MR, Mazoit J-X, Abdullah MA, Ghattas T, Crystal GJ (2014) The effectiveness of cricoid pressure for occluding the esophageal entrance in anesthetized and paralyzed patients: an experimental and observational glidescope study. Anesth Analg 118:580–586. https://doi.org/10.1213/ANE.0000000000000068
Eckardt AJ, Eckardt VF (2011) Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol 8:311–319. https://doi.org/10.1038/nrgastro.2011.68
Funding
No specific grants from any funding agencies in the public, commercial, or not-for-profit sectors were received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Oscar Santes, Enrique Coss-Adame, Miguel A. Valdovinos, Janette Furuzawa-Carballeda, Angélica Rodríguez-Garcés, Jose Peralta-Figueroa, Sofia Narvaez-Chavez, Hector Olvera-Prado, Uriel Clemente-Gutiérrez and Gonzalo Torres-Villalobos have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Santes, O., Coss-Adame, E., Valdovinos, M.A. et al. Does laparoscopic reoperation yield symptomatic improvements similar to those of primary laparoscopic Heller myotomy in achalasia patients?. Surg Endosc 35, 4991–5000 (2021). https://doi.org/10.1007/s00464-020-07978-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07978-7