Abstract
Background
Device-related interruptions in the operating room (OR) may create stress among health care providers and delays. Although non-technical skills (NTS) of the OR teams, such as situational awareness and communication, are expected to influence device-related interruptions, empirical data on this relationship are limited.
Methods
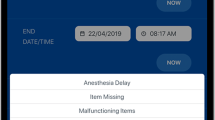
We performed a prospective cohort study of 144 consecutive elective laparoscopic operations during 13 months. A data capture system called the OR Black Box® was used to characterize device-related interruptions, NTS, and distractions. Device-related interruptions were classified according to a priori established categories. Positive and negative NTS instances were identified according to validated measurement tools specific for nurses and surgeons. We assessed the relationship between NTS and device-related interruptions after adjusting for potential confounders.
Results
A total of 86 device-related interruptions occurred in 48 of 144 operations (33%). They were most frequently classified as device failure (54%) followed by improper assembly (19%) and disconnection (14%). Medians of 1 [interquartile range (IQR) 0–3] and 1 (IQR 0–2) negative NTS instance per operation were demonstrated by nurses and surgeons, respectively. Medians of 28 (IQR 15–38) and 40 (IQR 28–118) positive NTS instances per operation were demonstrated by nurses and surgeons. In a multivariable analysis, a higher frequency of negative NTS instances demonstrated by nurses was associated with device-related interruptions after risk adjustment (Odds Ratio 1.33, p = 0.02).
Conclusions
In elective laparoscopic operations, an increased likelihood of device-related interruptions in the OR was associated with more frequent negative NTS demonstrations by nursing teams.
Similar content being viewed by others
References
Helmreich RL, Merritt AC, Wilhelm JA (1999) The evolution of crew resource management training in commercial aviation. Int J Aviat Psychol 9:19–32
Sexton JB, Thomas EJ, Helmreich RL (2000) Error, stress, and teamwork in medicine and aviation: cross sectional surveys. BMJ 320:745–749. https://doi.org/10.1136/bmj.320.7237.745
Barach P, Small SD (2000) Reporting and preventing medical mishaps: lessons from non-medical near miss reporting systems. BMJ 320:759–763. https://doi.org/10.1136/bmj.320.7237.759
Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM (2007) Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surg 142:658–665. https://doi.org/10.1016/j.surg.2007.07.034
Arora S, Hull L, Sevdalis N, Tierney T, Nestel D, Woloshynowych M, Darzi A, Kneebone R (2010) Factors compromising safety in surgery: stressful events in the operating room. Am J Surg 199:60–65. https://doi.org/10.1016/j.amjsurg.2009.07.036
von Strauss und Torney M, Dell-Kuster S, Hoffmann H, von Holzen U, Oertli D, Rosenthal R (2016) Microcomplications in laparoscopic cholecystectomy: impact on duration of surgery and costs. Surg Endosc 30:2512–2522. https://doi.org/10.1007/s00464-015-4512-3
Blikkendaal MD, Driessen SRC, Rodrigues SP, Rhemrev JPT, Smeets MJGH, Dankelman J, van den Dobbelsteen JJ, Jansen FW (2017) Surgical flow disturbances in dedicated minimally invasive surgery suites: an observational study to assess its supposed superiority over conventional suites. Surg Endosc 31:288–298. https://doi.org/10.1007/s00464-016-4971-1
Weerakkody RA, Cheshire NJ, Riga C, Lear R, Hamady MS, Moorthy K, Darzi AW, Vincent C, Bicknell CD (2013) Surgical technology and operating-room safety failures: a systematic review of quantitative studies. BMJ Qual Saf 22:710–718
Duff SN, Windham TC, Wiegmann DA, Kring J, Schaus JD, Malony R, Boquet A (2010) Identification and classification of flow disruptions in the operating room during two types of general surgery procedures. Proc Hum Factors Ergon Soc Annu Meet. https://doi.org/10.1177/154193121005401217
Healey AN, Sevdalis N, Vincent CA (2006) Measuring intra-operative interference from distraction and interruption observed in the operating theatre. Ergonomics 49:589–604. https://doi.org/10.1080/00140130600568899
Verdaasdonk EGG, Stassen LPS, van der Elst M, Karsten TM, Dankelman J (2007) Problems with technical equipment during laparoscopic surgery: an observational study. Surg Endosc 21:275–279. https://doi.org/10.1007/s00464-006-0019-2
Antoniadis S, Passauer-Baierl S, Baschnegger H, Weigl M (2014) Identification and interference of intraoperative distractions and interruptions in operating rooms. J Surg Res 188:21–29. https://doi.org/10.1016/j.jss.2013.12.002
Safety at the sharp end: a guide to non-technical skills. In: CRC Press. https://www.crcpress.com/Safety-at-the-Sharp-End-A-Guide-to-Non-Technical-Skills/Flin-OConnor/p/book/9780754646006. Accessed 20 Aug 2019
Yule S, Flin R, Maran N, Rowley D, Youngson G, Paterson-Brown S (2008) Surgeons’ non-technical skills in the operating room: reliability testing of the NOTSS behavior rating system. World J Surg 32:548–556. https://doi.org/10.1007/s00268-007-9320-z
Mitchell L (2017) Scrub practitioners’ list of intra-operative non-technical skills–SPLINTS. In: Flin R (ed) Safer surgery, 1st edn. CRC Press, Boca Raton, pp 67–81
Jung JJ, Borkhoff CM, Jüni P, Grantcharov TP (2018) Non-technical skills for surgeons (NOTSS): critical appraisal of its measurement properties. Am J Surg 216:990–997. https://doi.org/10.1016/j.amjsurg.2018.02.021
Jung JJ, Jüni P, Lebovic G, Grantcharov T (2018) First-year analysis of the operating room Black Box study. Ann Surg. https://doi.org/10.1097/SLA.0000000000002863
Jung JJ, Jüni P, Lebovic G, Grantcharov T (2020) First-year analysis of the operating room Black Box study. Ann Surg 271:122–127. https://doi.org/10.1097/SLA.0000000000002863
Fecso AB, Kuzulugil SS, Babaoglu C, Bener AB, Grantcharov TP (2018) Relationship between intraoperative non-technical performance and technical events in bariatric surgery. Br J Surg 105:1044–1050. https://doi.org/10.1002/bjs.10811
Jung JJ, Yule S, Boet S, Szasz P, Schulthess P, Grantcharov T (2020) Nontechnical skill assessment of the collective surgical team using the Non-Technical Skills for Surgeons (NOTSS) system. Ann Surg. https://doi.org/10.1097/SLA.0000000000003250
Sevdalis N, Forrest D, Undre S, Darzi A, Vincent C (2008) Annoyances, disruptions, and interruptions in surgery: the Disruptions in Surgery Index (DiSI). World J Surg 32:1643–1650. https://doi.org/10.1007/s00268-008-9624-7
Jung JJ, Elfassy J, Grantcharov T (2019) Factors associated with surgeon’s perception of distraction in the operating room. Surg Endosc. https://doi.org/10.1007/s00464-019-07088-z
Jung JJ, Kashfi A, Sharma S, Grantcharov T (2019) Characterization of device-related interruptions in minimally invasive surgery: need for intraoperative data and effective mitigation strategies. Surg Endosc 33:717–723. https://doi.org/10.1007/s00464-018-6254-5
Halverson AL, Casey JT, Andersson J, Anderson K, Park C, Rademaker AW, Moorman D (2011) Communication failure in the operating room. Surgery 149:305–310. https://doi.org/10.1016/j.surg.2010.07.051
Gillespie BM, Harbeck E, Kang E, Steel C, Fairweather N, Chaboyer W (2017) Correlates of non-technical skills in surgery: a prospective study. BMJ Open 7:e014480. https://doi.org/10.1136/bmjopen-2016-014480
Koh RYI, Park T, Wickens CD (2014) An investigation of differing levels of experience and indices of task management in relation to scrub nurses’ performance in the operating theatre: analysis of video-taped caesarean section surgeries. Int J Nurs Stud 51:1230–1240. https://doi.org/10.1016/j.ijnurstu.2014.01.005
Stubbings L, Chaboyer W, McMurray A (2012) Nurses’ use of situation awareness in decision-making: an integrative review. J Adv Nurs. https://doi.org/10.1111/j.1365-2648.2012.05989.x
Gillespie BM, Chaboyer W, Wallis M, Chang HA, Werder H (2009) Operating theatre nurses’ perceptions of competence: a focus group study. J Adv Nurs 65:1019–1028. https://doi.org/10.1111/j.1365-2648.2008.04955.x
Rosenorn-Lanng D (2015) Human factors in healthcare: level two. OUP, Oxford
Gillespie BM, Gwinner K, Fairweather N, Chaboyer W (2013) Building shared situational awareness in surgery through distributed dialog. J Multidiscip Healthc 6:109–118. https://doi.org/10.2147/JMDH.S40710
Hu Y-Y, Arriaga AF, Peyre SE, Corso KA, Roth EM, Greenberg CC (2012) Deconstructing intraoperative communication failures. J Surg Res 177:37–42. https://doi.org/10.1016/j.jss.2012.04.029
Moss J, Xiao Y (2004) Improving operating room coordination: communication pattern assessment. J Nurs Admin 34:93–100. https://doi.org/10.1097/00005110-200402000-00008
Sevdalis N, Wong HWL, Arora S, Nagpal K, Healey A, Hanna GB, Vincent CA (2012) Quantitative analysis of intraoperative communication in open and laparoscopic surgery. Surg Endosc 26:2931–2938. https://doi.org/10.1007/s00464-012-2287-3
Sonoda Y, Onozuka D, Hagihara A (2018) Factors related to teamwork performance and stress of operating room nurses. J Nurs Manag 26:66–73. https://doi.org/10.1111/jonm.12522
Kang E, Massey D, Gillespie BM (2015) Factors that influence the non-technical skills performance of scrub nurses: a prospective study. J Adv Nurs 71:2846–2857. https://doi.org/10.1111/jan.12743
Catchpole KR, Giddings AEB, Hirst G, Dale T, Peek GJ, de Leval MR (2008) A method for measuring threats and errors in surgery. Cogn Technol Work 10:295–304. https://doi.org/10.1007/s10111-007-0093-9
Catchpole K, Mishra A, Handa A, McCulloch P (2008) Teamwork and error in the operating room: analysis of skills and roles. Ann Surg 247:699–706. https://doi.org/10.1097/SLA.0b013e3181642ec8
Fletcher G, Flin R, McGeorge P, Glavin R, Maran N, Patey R (2003) Anaesthetists’ Non-Technical Skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth 90:580–588. https://doi.org/10.1093/bja/aeg112
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Teodor Grantcharov holds intellectual property ownership of Surgical Safety Technologies Inc. and is supported by research grants from Medtronic Canada, Ethicon Canada, Baxter Canada, Olympus Canada, Takeda Canada, and Intuitive Surgical. Dr. James J. Jung and Mr. Sahil Sharma have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sharma, S., Grantcharov, T. & Jung, J.J. Non-technical skills and device-related interruptions in minimally invasive surgery. Surg Endosc 35, 4494–4500 (2021). https://doi.org/10.1007/s00464-020-07962-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07962-1