Abstract
Background
There are no studies examining the use of subhepatic drains after simultaneous resection of synchronous colorectal liver metastases (sCRLM). This study aimed to (1) describe the current practices regarding primary drain placement, (2) evaluate drain efficacy in mitigating postoperative complications, and (3) determine impact of drain maintenance duration on patient outcomes.
Methods
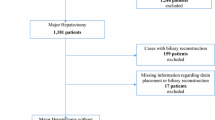
The ACS-NSQIP targeted data from 2014 to 2017 were analyzed. Propensity score of surgical drain versus no drain cohorts was performed. Main study outcomes were mortality, major morbidity, organ/space surgical site infection (SSI), secondary drain/aspiration procedure, and any septic events. Additional univariate/multivariate logistic analyses were performed to identify associations with drain placement and duration. Major hepatectomy was defined as formal right hepatectomy and any trisectionectomy.
Results
584 combined liver and colorectal resection (CRR) cases were identified. Open partial hepatectomy with colectomy was the most common procedure (70%, n = 407). Nearly 40% of patients received surgical drains (n = 226). Major hepatectomy, lower serum albumin, and no intraoperative portal vein occlusion (Pringle maneuver) were significantly associated with drain placement (p < 0.05). In the matched cohort (n = 190 in each arm), patients with surgical drains experienced higher rates of major morbidity (30% vs 12%), organ/space SSI (16% vs 6%), postoperative drain/aspiration procedures (9% vs 3%), and sepsis/septic shock (12% vs 4%) (all p < 0.05). Patients with severely prolonged drain removal, defined as after postoperative day 13 (POD13), had higher risk of postoperative morbidity compared to those with earlier drain removal (p < 0.01). 30-day mortality rate was not significantly different between the two groups.
Conclusion
Primary surgical drains were placed in a substantial percentage of patients undergoing combined resection for sCRLM. This case-matched analysis suggested that surgical drains are associated with an increase in postoperative morbidity. Postoperative drain maintenance past 13 days is associated with worse outcomes compared to earlier removal.



Similar content being viewed by others
References
Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, Bouvier AM (2006) Epidemiology and management of liver metastases from colorectal cancer. Ann Surg 244(2):254–259
Leporrier J, Maurel J, Chiche L, Bara S, Segol P, Launoy G (2006) A population-based study of the incidence, management and prognosis of hepatic metastases from colorectal cancer. Br J Surg 93(4):465–474
Martin RC 2nd, Augenstein V, Reuter NP, Scoggins CR, McMasters KM (2009) Simultaneous versus staged resection for synchronous colorectal cancer liver metastases. J Am Coll Surg 208(5):842–850. discussion 850–852
Shubert CR, Habermann EB, Bergquist JR, Thiels CA, Thomsen KM, Kremers WK, Kendrick ML, Cima RR, Nagorney DM (2015) A NSQIP review of major morbidity and mortality of synchronous liver resection for colorectal metastasis stratified by extent of liver resection and type of colorectal resection. J Gastrointest Surg 19(11):1982–1994
Silberhumer GR, Paty PB, Denton B, Guillem J, Gonen M, Araujo RLC, Nash GM, Temple LK, Allen PJ, DeMatteo RP, Weiser MR, Wong WD, Jarnagin WR, D'Angelica MI, Fong Y (2016) Long-term oncologic outcomes for simultaneous resection of synchronous metastatic liver and primary colorectal cancer. Surgery 160(1):67–73
Gurusamy KS, Samraj K, Davidson BR (2007) Routine abdominal drainage for uncomplicated liver resection. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD006232.pub2
Gavriilidis P, Hidalgo E, de'Angelis N, Lodge P, Azoulay D (2017) Re-appraisal of prophylactic drainage in uncomplicated liver resections: a systematic review and meta-analysis. HPB (Oxford) 19(1):16–20
Sun HC, Qin LX, Lu L, Wang L, Ye QH, Ren N, Fan J, Tang ZY (2006) Randomized clinical trial of the effects of abdominal drainage after elective hepatectomy using the crushing clamp method. Br J Surg 93(4):422–426
Burt BM, Brown K, Jarnagin W, DeMatteo R, Blumgart LH, Fong Y (2002) An audit of results of a no-drainage practice policy after hepatectomy. Am J Surg 184(5):441–445
Kim YI, Fujita S, Hwang VJ, Nagase Y (2014) Comparison of abdominal drainage and no-drainage after elective hepatectomy: a randomized study. Hepatogastroenterology 61(131):707–711
American College of Surgeons National Quality Improvement Program (2020). https://www.facs.org/quality-programs/acs-nsqip. Accessed 11 Apr 2020
Reddy SK, Barbas AS, Turley RS, Steel JL, Tsung A, Marsh JW, Geller DA, Clary BM (2011) A standard definition of major hepatectomy: resection of four or more liver segments. HPB (Oxford) 13(7):494–502
Austin PC (2011) Comparing paired vs non-paired statistical methods of analyses when making inferences about absolute risk reductions in propensity-score matched samples. Stat Med 30(11):1292–1301
Belghiti J, Kabbej M, Sauvanet A, Vilgrain V, Panis Y, Fekete F (1993) Drainage after elective hepatic resection. A randomized trial. Ann Surg 218(6):748–753
Squires MH 3rd, Lad NL, Fisher SB, Kooby DA, Weber SM, Brinkman A, Sarmiento JM, Scoggins CR, Egger ME, Cardona K, Cho CS, Martin RC, Russell MC, Winslow E, Staley CA 3rd, Maithel SK (2015) Value of primary operative drain placement after major hepatectomy: a multi-institutional analysis of 1,041 patients. J Am Coll Surg 220(4):396–402
Butte JM, Grendar J, Bathe O, Sutherland F, Grondin S, Ball CG, Dixon E (2014) The role of peri-hepatic drain placement in liver surgery: a prospective analysis. HPB (Oxford) 16(10):936–942
Jones TJ, Murphy AE, Tameron A, Hussain LR, Grannan K, Guend H, Dunki-Jacobs EM, Lee DY (2019) Trends and outcomes of synchronous resection of colorectal metastasis in the modern era-analysis of targeted hepatic NSQIP database. J Surg Res 238:35–40
Fagenson AM, Gleeson EM, Lau KKN, Karachristos A, Pitt HA (2020) Early drain removal after hepatectomy: an underutilized management strategy. HPB (Oxford). https://doi.org/10.1016/j.hpb.2020.03.005
Hirokawa F, Hayashi M, Miyamoto Y, Asakuma M, Shimizu T, Komeda K, Inoue Y, Tanigawa N (2011) Re-evaluation of the necessity of prophylactic drainage after liver resection. Am Surg 77(5):539–544
Inoue Y, Imai Y, Kawaguchi N, Hirokawa F, Hayashi M, Uchiyama K (2017) Management of abdominal drainage after hepatic resection. Dig Surg 34(5):400–410
Brauer DG, Nywening TM, Jaques DP, Doyle MB, Chapman WC, Fields RC, Hawkins WG (2016) Operative site drainage after hepatectomy: a propensity score matched analysis using the American College of Surgeons NSQIP targeted hepatectomy database. J Am Coll Surg 223(6):774–783 e2
Shwaartz C, Fields AC, Aalberg JJ, Divino CM (2017) Role of drain placement in major hepatectomy: a NSQIP analysis of procedure-targeted hepatectomy cases. World J Surg 41(4):1110–1118
Liu CL, Fan ST, Lo CM, Wong Y, Ng IO, Lam CM, Poon RT, Wong J (2004) Abdominal drainage after hepatic resection is contraindicated in patients with chronic liver diseases. Ann Surg 239(2):194–201
Moreno Elola-Olaso A, Davenport DL, Hundley JC, Daily MF, Gedaly R (2012) Predictors of surgical site infection after liver resection: a multicentre analysis using National Surgical Quality Improvement Program data. HPB (Oxford) 14(2):136–141
Noyes LD, Doyle DJ, McSwain NE Jr (1988) Septic complications associated with the use of peritoneal drains in liver trauma. J Trauma 28(3):337–346
Yamazaki S, Takayama T, Moriguchi M, Mitsuka Y, Okada S, Midorikawa Y, Nakayama H, Higaki T (2012) Criteria for drain removal following liver resection. Br J Surg 99(11):1584–1590
Hokuto D, Nomi T, Yasuda S, Kawaguchi C, Yoshikawa T, Ishioka K, Obara S, Yamada T, Kanehiro H (2017) The safety of the early removal of prophylactic drainage after liver resection based solely on predetermined criteria: a propensity score analysis. HPB (Oxford) 19(4):359–364
Mitsuka Y, Yamazaki S, Yoshida N, Masamichi M, Higaki T, Takayama T (2016) Prospective validation of optimal drain management "The 3 × 3 Rule" after liver resection. World J Surg 40(9):2213–2220
Pile JC (2006) Evaluating postoperative fever: a focused approach. Cleve Clin J Med 73(Suppl 1):S62–S66
Botrel TEA, Clark LGO, Paladini L, Clark OAC (2016) Efficacy and safety of bevacizumab plus chemotherapy compared to chemotherapy alone in previously untreated advanced or metastatic colorectal cancer: a systematic review and meta-analysis. BMC Cancer 16:677
Acknowledgements
The authors would like to thank Rodica Muraru and the Center for Outcomes Research in Surgery (CORES) department at the Indiana University School of Medicine for their contribution in providing statistical advice.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Yee, Al-Temimi, Flick, Nguyen, Zyromski, Schmidt, Nakeeb, House, Ceppa, and Mrs. Kilbane have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Hepatectomy CPT codes:
47120, 47122, 47125, 47130
Colectomy CPT codes:
44140, 44141, 44143, 44144, 44145, 44146, 44147, 44150, 44151, 44160, 44204, 44205, 44206, 44207, 44208, 44210
Proctectomy CPT codes:
44155, 44156, 44157, 44158, 44211, 44212, 45110, 45111, 45112, 45113, 45114, 45116, 45119, 45120, 45121, 45123, 45126, 45130, 45135, 45160, 45395, 45397, 45402, 45550
Secondary liver metastases ICD-9/10 codes:
C78.7, 197.
Rights and permissions
About this article
Cite this article
Yee, E.J., Al-Temimi, M.H., Flick, K.F. et al. Use of primary surgical drains in synchronous resection for colorectal liver metastases: a NSQIP analysis of current practice paradigm. Surg Endosc 35, 4275–4284 (2021). https://doi.org/10.1007/s00464-020-07917-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07917-6