Abstract
Background
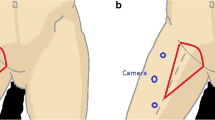
Conventional inguinal lymph node dissection comes with a high wound complication rate which increases hospital stay and may delay adjuvant treatment. Minimally invasive lymph node dissection (MILND) is a novel endoscopic technique which aims to minimize complications of lymphadenectomy. Herein we present our technique and experience with MILND to examine safety, feasibility and reproducibility in a setting of limited resources.
Methods
All patients undergoing MILND in the National Cancer Institute, Cairo were prospectively included following informed consent, IRB and ethical committee approval. Demographics, clinical, pathological data and postoperative complications according to Clavien–Dindo classification were recorded. Footage collected was used to create a step-by-step video demonstrating the technique.
Results
Twenty-seven procedures were included in the study. The most common indications were vulval cancer (44%) and skin melanoma (19%). There were 5 (18%) conversions to open procedure, all of them in the first 10 cases of the learning curve. The median (range) operative time was 120 (45–240) min and there was a trend towards shorter operative time after the first 5 cases. Wound dehiscence occurred in 4 cases (15%). Three of them (11%) required reoperation (grade III). Grade I/II complications in the form of seroma and wound infection occurred in 34%. The median (range) postoperative hospital stay was 2 (1–14). The median (range) number of retrieved lymph nodes was 12 (3–19). No grade III/IV lymphedema was recorded at 90 days after surgery.
Conclusion
MILND is a safe, feasible technique associated with relatively low postoperative wound complications even when performed in a centre with relatively limited resources.



Similar content being viewed by others
References
Chang SB, Askew RL, Xing Y, Weaver S, Gershenwald JE, Lee JE, Royal R, Lucci A, Ross MI, Cormier JN (2010) Prospective assessment of postoperative complications and associated costs following Inguinal Lymph Node Dissection (ILND) in Melanoma patients. Ann Surg Oncol 17:2764–2772
Spiess PE, Hernandez MS, Pettaway CA (2009) Contemporary inguinal lymph node dissection: minimizing complications. World J Urol 27:205–212. https://doi.org/10.1007/s00345-008-0324-6
Abbott AM, Grotz TE, Rueth NM, Hernandez Irizarry RC, Tuttle TM, Jakub JW (2013) Minimally invasive inguinal lymph node dissection (MILND) for melanoma: experience from two academic centers. Ann Surg Oncol 20:340–345. https://doi.org/10.1245/s10434-012-2545-6
Bishoff JT (2012) Endoscopic subcutaneous modified inguinal lymph node dissection for squamous cell carcinoma of the penis. Smith’s textbook endourology, 3rd edn, vol 2. pp 917–923. https://doi.org/10.1002/9781444345148.ch78
Tobias-Machado M, Tavares A, Silva MNR, Molina WR, Forseto PH, Juliano RV, Wroclawski ER (2008) Can video endoscopic inguinal lymphadenectomy achieve a lower morbidity than open lymph node dissection in penile cancer patients? J Endourol 22:1687–1691. https://doi.org/10.1089/end.2007.0386
Jakub JW, Terando AM, Sarnaik A, Ariyan CE, Faries MB, Zani S, Neuman HB, Wasif N, Farma JM, Averbook BJ, Bilimoria KY, Grotz TE, Allred JBJ, Suman VJ, Brady MS, Tyler D, Wayne JD, Nelson H (2017) Safety and feasibility of minimally invasive inguinal lymph node dissection in patients with melanoma (SAFE-MILND): report of a prospective multi-institutional trial. Ann Surg 265:192–196. https://doi.org/10.1097/SLA.0000000000001670
Jakub JW, Terando AM, Sarnaik A, Ariyan CE, Faries MB, Zani S, Neuman HB, Wasif N, Farma JM, Averbook BJ, Bilimoria KY, Allred JB, Suman VJ, Grotz TE, Zendejas B, Wayne JD, Tyler DS (2016) Training high-volume melanoma surgeons to perform a novel minimally invasive inguinal lymphadenectomy: report of a prospective multi-institutional trial. J Am Coll Surg 222:253–260. https://doi.org/10.1016/j.jamcollsurg.2015.11.010
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Executive Committee (2016) The diagnosis and treatment of peripheral lymphedema: 2016 consensus document of the International Society of Lymphology. Lymphology 49(4):170–184
Martin BM, Master VA, Delman KA (2013) Videoscopic inguinal lymphadenectomy for metastatic melanoma. Cancer Control 20:255–260. https://doi.org/10.1177/107327481302000403
Faries B, Thompson JF, Cochran AJ, Andtbacka RH, Mozzillo N, Zager JS, Jahkola T, Bowles TL, Testori A, Beitsch PD, Hoekstra HJ, Moncrieff M, Ingvar C, Wouters MWJM, Sabel MS, Levine EA, Agnese D, Henderson M, Dummer R, Rossi CR, Neves RI, Trocha SD, Wright F, Byrd DR, Matter M, Hsueh E, MacKenzie-Ross A, Johnson DB, Terheyden P, Berger AC, Huston TL, Wayne JD, Smithers BM, Neuman HB, Schneebaum S, Gershenwald JE, Ariyan CE, Desai DC, Jacobs L, McMasters KM, Gesierich A, Hersey P, Bines SD, Kane JM, Barth RJ, McKinnon G, Farma JM, Schultz E, Vidal-Sicart S, Hoefer RA, Lewis JM, Scheri R, Kelley MC, Nieweg OE, Noyes RD, Hoon DSB, Wang HJ, Elashoff DA, Elashoff RM (2017) Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med 376:2211–2222. https://doi.org/10.1056/NEJMoa1613210
Leiter U, Stadler R, Mauch C, Hohenberger W, Brockmeyer N, Berking C, Sunderkötter C, Kaatz M, Schulte KW, Lehmann P, Vogt T, Ulrich J, Herbst R, Gehring W, Simon JC, Keim U, Martus P, Garbe C (2016) Complete lymph node dissection versus no dissection in patients with sentinel lymph node biopsy positive melanoma (DeCOG-SLT): a multicentre, randomised, phase 3 trial. Lancet Oncol 17:757–767. https://doi.org/10.1016/S1470-2045(16)00141-8
Bartlett EK, Meise C, Bansal N, Fischer JP, Low DW, Czerniecki BJ, Roses RE, Fraker DL, Kelz RR, Karakousis GC (2013) Sartorius transposition during inguinal lymphadenectomy for melanoma. J Surg Res 184:209–215. https://doi.org/10.1016/j.jss.2013.04.033
Tauber R, Schmid S, Horn T, Thalgott M, Heck M, Haller B, Kübler H, Autenrieth M, Retz M, Gschwend JE, Maurer T (2013) Inguinal lymph node dissection: epidermal vacuum therapy for prevention of wound complications. J Plast Reconstr Aesthetic Surg 66:390–396. https://doi.org/10.1016/j.bjps.2012.09.030
Sarnaik AA, Puleo CA, Zager JS, Sondak VK (2009) Limiting the morbidity of inguinal lymphadenectomy for metastatic melanoma. Cancer Control 16:240–247. https://doi.org/10.1177/107327480901600306
Tobias-Machado M, Tavares A, Ornellas AA, Molina WR, Juliano RV, Wroclawski ER (2007) Video endoscopic inguinal lymphadenectomy: a new minimally invasive procedure for radical management of inguinal nodes in patients with penile squamous cell carcinoma. J Urol 177:953–958. https://doi.org/10.1016/j.juro.2006.10.075
Tobias-Machado M, Tavares A, Molina WR, Forseto PH, Juliano RV, Wroclawski ER (2006) Video endoscopic inguinal lymphadenectomy (VEIL): minimally invasive resection of inguinal lymph nodes. Int Braz J Urol 32:316–321. https://doi.org/10.1590/S1677-55382006000300012
Delman KA, Kooby DA, Rizzo M, Ogan K, Master V (2011) Initial experience with videoscopic inguinal lymphadenectomy. Ann Surg Oncol 18:977–982. https://doi.org/10.1245/s10434-010-1490-5
Martin BM, Etra JW, Russell MC, Rizzo M, Kooby DA, Staley CA, Master VA, Delman KA (2014) Oncologic outcomes of patients undergoing Videoscopic inguinal lymphadenectomy for metastatic melanoma. J Am Coll Surg 218:620–626. https://doi.org/10.1016/j.jamcollsurg.2013.12.016
Lasithiotakis K, Maurichi A, Santinami M, Zoras O (2017) The advent of minimally invasive lymphadenectomy in melanoma. Ann Laparosc Endosc Surg 2:122. https://doi.org/10.21037/ales.2017.06.14
Postlewait LM, Farley CR, Seamens AM, Le N, Rizzo M, Russell MC, Lowe MC, Delman KA (2018) Morbidity and outcomes following axillary lymphadenectomy for melanoma: weighing the risk of surgery in the era of MSLT-II. Ann Surg Oncol 25:465–470. https://doi.org/10.1245/s10434-017-6242-3
Kumar V, Sethia KK (2017) Prospective study comparing video-endoscopic radical inguinal lymph node dissection (VEILND) with open radical ILND (OILND) for penile cancer over an 8-year period. BJU Int 119:530–534. https://doi.org/10.1111/bju.13660
Li M, Wang S, Guo S, Zhang Z (2015) Endoscopic groin lymphadenectomy with a thigh approach to gynecologic malignancies: a retrospective study with 5-year experience. Int J Gynecol Cancer 25:325–330. https://doi.org/10.1097/IGC.0000000000000348
Postlewait LM, Farley CR, Diller ML, Martin B, Hart Squires M, Russell MC, Rizzo M, Ogan K, Master V, Delman K (2017) A minimally invasive approach for inguinal lymphadenectomy in melanoma and genitourinary malignancy: long-term outcomes in an attempted randomized control trial. Ann Surg Oncol 24:3237–3244. https://doi.org/10.1245/s10434-017-5971-7
Stuiver MM, Westerduin E, Ter Meulen S, Vincent AD, Nieweg OE, Wouters MWJM (2014) Surgical wound complications after groin dissection in melanoma patients—a historical cohort study and risk factor analysis. Eur J Surg Oncol 40:1284–1290. https://doi.org/10.1016/j.ejso.2014.01.019
Stuiver MM, Djajadiningrat RS, Graafland NM, Vincent AD, Lucas C, Horenblas S (2013) Early wound complications after inguinal lymphadenectomy in penile cancer: a historical cohort study and risk-factor analysis. Eur Urol 64:486–492. https://doi.org/10.1016/j.eururo.2013.02.037
Master VA, Jafri SMA, Moses KA, Ogan K, Kooby DA, Delman KA (2012) Minimally invasive inguinal lymphadenectomy via endoscopic groin dissection: comprehensive assessment of immediate and long-term complications. J Urol 188:1176–1180. https://doi.org/10.1016/j.juro.2012.06.038
Pahwa HS, Misra S, Kumar A, Kumar V, Agarwal A, Srivastava R (2013) Video Endoscopic Inguinal Lymphadenectomy (VEIL)—a prospective critical perioperative assessment of feasibility and morbidity with points of technique in penile carcinoma. World J Surg Oncol 11:2–7. https://doi.org/10.1186/1477-7819-11-42
Contreras N, Jakub JW (2020) The achilles heel of minimally invasive inguinal lymph node dissection: seroma formation: Seroma MILND. Am J Surg 219:696–700. https://doi.org/10.1016/j.amjsurg.2019.06.010
Sommariva A, Pasquali S, Cona C, Ciccarese AA, Saadeh L, Campana LG, Meroni M, Rossi CR (2016) Videoscopic ilioinguinal lymphadenectomy for groin lymph node metastases from melanoma. Br J Surg 103:1026–1031. https://doi.org/10.1002/bjs.10140
Gerken ALH, Dobroschke J, Reißfelder C, Hetjens S, Braun V, Di Monta G, Jakob J, Hohenberger P, Nowak K, Herrle F (2019) Tissue sealants for the prevention of lymphoceles after radical inguinal lymph node dissection in patients with melanoma: a systematic review and individual patient data meta-analysis. J Surg Oncol 119:728–736. https://doi.org/10.1002/jso.25366
Bell JG, Lea JS, Reid GC (2000) Complete groin lymphadenectomy with preservation of the fascia lata in the treatment of vulvar carcinoma. Gynecol Oncol 77:314–318. https://doi.org/10.1006/gyno.2000.5790
Zhang X, Sheng X, Niu J, Li H, Li D, Tang L, Li Q, Li Q (2007) Sparing of saphenous vein during inguinal lymphadenectomy for vulval malignancies. Gynecol Oncol 105:722–726. https://doi.org/10.1016/j.ygyno.2007.02.011
Chuo CB, Srivastava S (2010) Management of groin seromas with external quilting sutures and open drainage. J Plast Reconstr Aesthetic Surg 63:e551–e552. https://doi.org/10.1016/j.bjps.2009.12.009
Chen D, Li Z, Song J, Zheng X, Yu A (2016) Systematic review and meta-analysis of the use of quilting to prevent seroma formation after axillary lymphadenectomy. Int J Clin Exp Med 9:760–772
Grotz TE, Huebner M, Pockaj BA, Perkins S, Jakub JW (2013) Limitations of lymph node ratio, evidence-based benchmarks, and the importance of a thorough lymph node dissection in melanoma. Ann Surg Oncol 20:4370–4377. https://doi.org/10.1245/s10434-013-3186-0
Rossi CR, Mozzillo N, Maurichi A, Pasquali S, Quaglino P, Borgognoni L, Solari N, Piazzalunga D, Mascheroni L, Giudice G, Mocellin S, Patuzzo R, Caracò C, Ribero S, Marone U, Santinami M (2014) The number of excised lymph nodes is associated with survival of melanoma patients with lymph nodemetastasis. Ann Oncol 25:240–246. https://doi.org/10.1093/annonc/mdt510
Spillane AJ, Haydu L, McMillan W, Stretch JR, Thompson JF (2011) Quality assurance parameters and predictors of outcome for ilioinguinal and inguinal dissection in a contemporary melanoma patient population. Ann Surg Oncol 18:2521–2528. https://doi.org/10.1245/s10434-011-1755-7
Morton DL, Thompson JF, Cochran AJ, Mozzillo N, Nieweg OE, Roses DF, Hoekstra HJ, Karakousis CP, Puleo CA, Coventry BJ, Kashani-Sabet M, Smithers BM, Paul E, Kraybill WG, McKinnon JG, Wang HJ, Elashoff R, Faries MB (2014) Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med 370:599–609. https://doi.org/10.1056/NEJMoa1310460
Egger ME, Brown RE, Roach BA, Quillo AR, Martin RCG, Scoggins CR, Stromberg AJ, McMasters KM (2014) Addition of an iliac/obturator lymph node dissection does not improve nodal recurrence or survival in melanoma. J Am Coll Surg 219:101–108. https://doi.org/10.1016/j.jamcollsurg.2014.02.019
Romanelli P, Nishimoto R, Suarez R, Decia R, Abreu D, Machado M, Arroyo C, Campolo H, Campos E, Carlos AS, Tobias-Machado M (2013) Video endoscopic inguinal lymphadenectomy: Surgical and oncological results. Actas Urológicas Españolas (English Ed 37:305–310). https://doi.org/10.1016/j.acuroe.2012.11.005
Zendejas B, Jakub JW, Terando AM, Sarnaik A, Ariyan CE, Faries MB, Zani S, Neuman HB, Wasif N, Farma JM, Averbook BJ, Bilimoria KY, Tyler D, Brady MS, Farley DR (2017) Laparoscopic skill assessment of practicing surgeons prior to enrollment in a surgical trial of a new laparoscopic procedure. Surg Endosc 31:3313–3319. https://doi.org/10.1007/s00464-016-5364-1
Acknowledgements
I cannot express enough my gratitude to Dr. Waheed Yosry Gareer, Dr. Sherif Maamoun, Dr. Ahmed Morsy, Dr. Samy Ramzy and Dr. Hisham Anwar for their invaluable clinical support, Dr. Inas Elattar for helping with statistics, Adham Bakry and Lorena Mora for helping with illustrations, Begad Omran for helping with the video, and Dr. Paul Sugarbaker and Dr Charles Balch for their mentoring.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Hisham Abdel Mageed, Dr. Ihab Saad, Dr. Tarek Elbaradie, Dr. Ahmed Mostafa, Dr. Mohammed Safa, Dr. Mohammed Gamil and Dr. Konstantinos Lasithiotakis have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary video
Rights and permissions
About this article
Cite this article
Abdel Mageed, H., Saad, I., Mostafa, A. et al. Minimally invasive inguinal lymph node dissection: initial experience and reproducibility in a limited resource setting—with technique video. Surg Endosc 34, 4669–4676 (2020). https://doi.org/10.1007/s00464-020-07813-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07813-z