Abstract
Background and aims
At specialized facilities, endoscopic submucosal dissection (ESD) has currently been performed even for difficult cases such as tumors extending to a diverticulum that previously required surgery. This study aims to classify the type of lesion according to the degree of infiltration to a diverticulum and assessed the safety and efficacy of ESD for each type of lesion.
Methods
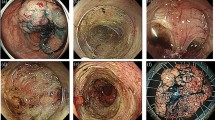
We retrospectively reviewed ESD for lesions at NTT Medical Center Tokyo between January 2014 and April 2019. Lesions were classified as follows: Type 1: lesions in contact with or within 3 mm of the edge of a diverticulum; Type 2: lesions that partially infiltrated into a diverticulum; and Type 3: lesions that infiltrated into and completely covered the diverticulum. Furthermore, ESD strategies were divided into A and B, which indicates that a lesion was resected separately from the diverticulum and along the entire diverticulum, respectively. The clinicopathological characteristics and clinical outcomes were analyzed according to the strategy.
Results
A total of 47 lesions satisfied inclusion criteria (19 Type 1, 12 Type 2, and 16 Type 3 lesions). 19 Type 1 and 8 Type 2 lesions were resected using Strategy A, while 4 Type 2 and 16 Type 3 lesions were resected using Strategy B. En bloc resection was achieved in all cases. In Strategy A, the R0 resection rate was 96.3% and the curative resection rate was 88.9%. On the contrary, in Strategy B, the R0 resection rate was 95.0% and the curative resection rate was 90.0%. In Strategy B, one of the patients developed post-operative bleeding that required endoscopic hemostasis; another patient developed delayed perforation that required emergency surgery.
Conclusions
ESD for colorectal neoplasms in proximity or extending to a diverticulum is challenging, but this procedure can be a safe and effective therapeutic option.






Similar content being viewed by others
References
Fujishiro M, Yahagi N, Kakushima N et al (2007) Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol 5:678–683
Terasaki M, Tanaka S, Oka S et al (2012) Clinical outcomes of endoscopic submucosal dissection and endoscopic mucosal resection for laterally spreading tumors larger than 20 mm. J Gastroenterol Hepatol 27(4):734–740
Niimi K, Fujishiro M, Kodashima S et al (2010) Long-term outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 42(9):723–729
Hori K, Uraoka T, Harada K et al (2014) Predictive factors for technically difficult endoscopic submucosal dissection in the colorectum. Endoscopy 46:862–870
Tanaka S, Oka S, Kaneko I et al (2007) Endoscopic submucosal dissection for colorectal neoplasia: possibility of standardization. Gastrointest Endosc 66:100–107
Saito Y, Uraoka T, Yamaguchi Y et al (2010) A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 72:1217–1225
Ohata K, Nonaka K, Misumi Y et al (2016) Usefulness of training using animal models for colorectal endoscopic submucosal dissection: is experience performing gastric ESD really needed? Endosc Int Open 4(3):E333–E339
Cao Y, Liao C, Tan A et al (2009) Meta-analysis of endoscopic submucosal dissection versus endoscopic mucosal resection for tumors of the gastrointestinal tract. Endoscopy 41(9):751–757
Draganov PV, Gotoda T, Chavalitdhamrong D et al (2013) Techniques of endoscopic submucosal dissection: application for the Western endoscopist? Gastrointest Endosc 78(5):677–688
Antillon MR, Bartalos CR, Miller ML et al (2008) En bloc endoscopic submucosal dissection of a 14-cm laterally spreading adenoma of the rectum with involvement to the anal canal: expanding the frontiers of endoscopic surgery (with video). Gastrointest Endosc 67(2):332–337
Hurlstone DP, Atkinson R, Sanders DS et al (2007) Achieving R0 resection in the colorectum using endoscopic submucosal dissection. Br J Surg 94(12):1536–1542
Sato K, Ito S, Kitagawa T et al (2014) Factors affecting the technical difficulty and clinical outcome of endoscopic submucosal dissection for colorectal tumors. Surg Endosc 28:2959–2965
Takeuchi Y, Iishi H, Tanaka S et al (2014) Factors associated with technical difficulties and adverse events of colorectal endoscopic submucosal dissection: retrospective exploratory factor analysis of a multicenter prospective cohort. Int J Colorectal Dis 29:1275–1284
Imai K, Hotta K, Yamaguchi Y et al (2016) Preoperative indicators of failure of en bloc resection or perforation in colorectal endoscopic submucosal dissection: implication for lesion stratification by technical difficulties during stepwise training. Gastrointest Endosc 83(5):954–962
Takasago T, Kuwai T, Yamaguchi T et al (2017) Endoscopic submucosal dissection with a scissors-type knife for post-EMR recurrence tumor involving the colon diverticulum. VideoGIE 2(8):211–212
Iwatsubo T, Uedo N, Yamasaki Y et al (2017) Traction-assisted colorectal endoscopic submucosal dissection by use of clip and line for a neoplasm involving colonic diverticulum. VideoGIE 2(12):337–338
Jimenez-Garcia VA, Yamada M, Ikematsu H et al (2019) Endoscopic submucosal dissection in management of colorectal tumors near or involving a diverticulum: a retrospective case series. Endosc Int Open 7(5):E664–E671
Kudo S, Tamura S, Nakajima T et al (1996) Diagnosis of colorectal tumorous lesions by magnifying endoscopy. Gastrointest Endosc 44(1):8–14
Kudo S, Tamegai Y, Yamano H et al (2001) Endoscopic mucosal resection of the colon: the Japanese technique. Gastrointest Endosc Clin N Am 11(3):519–535
Matsuda T, Fujii T, Saito Y et al (2008) Efficacy of the invasive/non-invasive pattern by magnifying chromoendoscopy to estimate the depth of invasion of early colorectal neoplasms. Am J Gastroenterol 103:2700–2706
Kita H, Yamamoto H, Miyata T et al (2007) Endoscopic submucosal dissection using sodium hyaluronate, a new technique for en bloc resection of a large superficial tumor in the colon. Inflammopharmacology 15:129–131
Schlemper RJ, Riddell RH, Kato Y et al (2000) The Vienna classification of gastrointestinal epithelial neoplasia. Gut 47(2):251–255
Dixon MF (2002) Gastrointestinal epithelial neoplasia: Vienna revisited. Gut 51(1):130–131
Watanabe T, Itabashi M, Shimada Y et al (2015) Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol 20(2):207–239
Peery AF, Barrett PR, Park D et al (2012) A high-fiber diet does not protect against asymptomatic diverticulosis. Gastroenterology 142:266–272
Peery AF, Keku TO, Martin CF et al (2016) Distribution and characteristics of colonic diverticula in a United States screening population. Clin Gastroenterol Hepatol 14:980–985
Yamamichi N, Shimamoto T, Takahashi Y et al (2015) Trend and risk factors of diverticulosis in Japan: age, gender, and lifestyle/metabolic-related factors may cooperatively affect on the colorectal diverticula formation. PLoS ONE 10:e0123688. https://doi.org/10.1371/journal.pone.0123688
Ritsuno H, Sakamoto N, Osada T et al (2015) Large superficial tumor of the colon involving a diverticulum removed by endoscopic submucosal dissection. Gastrointest Endosc 82:751
Kato M, Uraoka T, Wada M et al (2016) Laterally spreading tumor involving a colon diverticulum successfully resected by endoscopic submucosal dissection. Gastrointest Endosc 84:191–192
Iwatsubo T, Uedo N, Yamasaki Y et al (2017) Traction-assisted colorectal endoscopic submucosal dissection by use of clip and line for a neoplasm involving colonic diverticulum. VideoGIE 2:337–338
Mori H, Kobara H, Nishiyama N et al (2017) Novel effective and repeatedly available ring-thread counter traction for safer colorectal endoscopic submucosal dissection. Surg Endosc 31(7):3040–3047
Meyers MA, Alonso DR, Gray GF et al (1976) Pathogenesis of bleeding colonic diverticulosis. Gastroenterology 71(4):577–583
Tashima T, Ohata K, Sakai E et al (2018) Efficacy of an over-the-scope clip for preventing adverse events after duodenal endoscopic submucosal dissection: a prospective interventional study. Endoscopy 50(5):487–496
Carmo J, Marques S, Chapim I et al (2015) Elastic band ligation for the removal of a colonic tubular adenoma in a diverticulum. Endoscopy. 47:E490–E491
Pinho R, Oliveira M, Mascarenhas-Saraiva M (2015) Endoscopic full-thickness resection of an inverted colonic diverticulum with intraepithelial neoplasia using the ligate-and-let-go technique. Clin Gastroenterol Hepatol 13:A33–A34
Shakhatreh MH, Hair C, Shaib YH et al (2015) Removal of a colonic polyp in a diverticulum: a novel use of the over-the-scope clip device. Gastrointest Endosc 81:756
Valli PV, Kaufmann M, Vrugt B et al (2014) Endoscopic resection of a diverticulum-arisen colonic adenoma using a full-thickness resection device. Gastroenterology 147:969–971
Fu KI, Hamahata Y, Tsujinaka Y (2010) Early colon cancer within a diverticulum treated by magnifying chromoendoscopy and laparoscopy. World J Gastroenterol 16:1545–1547
Kajiwara H, Umemura S, Mukai M et al (1996) Adenocarcinoma arising within a colonic diverticulum. Pathol Int 46:538–539
Takasago T, Kuwai T, Yamaguchi T et al (2017) Endoscopic submucosal dissection with a scissors-type knife for post-EMR recurrence tumor involving the colon diverticulum. VideoGIE 2:211–212
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Takashi Muramoto, Ken Ohata, Eiji Sakai, Syunya Takayanagi, Yoshiaki Kimoto, Yuichiro Suzuki, Rindo Ishii, Keisuke Kanda, Ryoju Negishi, Maiko Takita, Yohei Minato, Yosuke Tsuji, Hideyuki Chiba and Nobuyuki Matsuhashi have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muramoto, T., Ohata, K., Sakai, E. et al. Endoscopic submucosal dissection for colorectal neoplasms in proximity or extending to a diverticulum. Surg Endosc 35, 3479–3487 (2021). https://doi.org/10.1007/s00464-020-07795-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07795-y