Abstract
Background
The majority of laparoscopic paraesophageal hernia (PEH) repairs are performed electively. We aimed to investigate the frequency of non-elective laparoscopic (MIS) PEH repair and compare 30-day outcomes to elective MIS repairs and non-elective open repairs. We hypothesized that an increasing percentage of non-elective PEH repairs would be performed laparoscopically and that this population would have improved outcomes compared to non-elective open PEH counterparts.
Methods
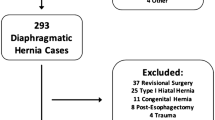
The 2011–2016 NSQIP PUFs were used to identify patients who underwent PEH repair. Case status was classified as open vs. MIS and elective versus non-elective. Preoperative patient characteristics, operative details, discharge destination, and 30-day postoperative complication rates were compared. Logistic regression was used to examine the impact of case status on 30-day mortality.
Results
We identified 20,010 patients who underwent PEH. There were an increasing number of MIS PEH repairs in NSQIP between 2011 and 2016. Non-elective repairs were performed in 2,173 patients and 73.4% of these were completed laparoscopically. Elective MIS patients were younger, had a higher BMI, and were more likely to be functionally independent (p < 0.01) than their non-elective counterparts. Non-elective MIS patients had a higher wound class and ASA class compared to their elective counterparts. Compared to elective MIS cases, non-elective MIS PEH repair was associated with increased odds of mortality, even after controlling for patient characteristics (OR = 1.76, p = 0.02). There was no statistically significant difference in mortality for non-elective MIS vs. non-elective open PEH repair. There is an increase in non-elective PEH repairs recorded in NSQIP over time studied.
Conclusions
The population undergoing non-elective MIS PEH repairs is different from their elective MIS counterparts and experience a higher postoperative mortality rate. While the observed increased utilization of MIS techniques in non-elective PEH repairs likely provides benefits for the patient, there remain differences in outcomes for these patients compared to elective PEH repairs.
Similar content being viewed by others
References
Mungo B, Molena D, Stem M, Feinberg RL, Lidor AO (2014) Thirty-day outcomes of paraesophageal hernia repair using the NSQIP database: should laparoscopy be the standard of care? J Am Coll Surg 219:229–236. https://doi.org/10.1016/J.JAMCOLLSURG.2014.02.030
Quinn MA, Geraghty AJ, Robertson AGN, Paterson-Brown S, Lamb PJ, Group the EO-GS (2019) Long-term outcomes following surgical repair of giant paraoesophageal hiatus hernia. Surg Endosc 33:1846–1853. https://doi.org/10.1007/s00464-018-6463-y
Teague WJ, Ackroyd R, Watson DI, Devitt PG (2000) Changing patterns in the management of gastric volvulus over 14 years. Br J Surg 87:358–361. https://doi.org/10.1046/j.1365-2168.2000.01385.x
Malangoni MA, Biester TW, Jones AT, Klingensmith ME, Lewis FR (2013) Operative experience of surgery residents: trends and challenges. J Surg Educ 70:783–788. https://doi.org/10.1016/J.JSURG.2013.09.015
Dominguez EP, Barrat C, Shaffer L, Gruner R, Whisler D, Taylor P (2013) Minimally invasive surgery adoption into an established surgical practice: impact of a fellowship-trained colleague. Surg Endosc 27:1267–1272. https://doi.org/10.1007/s00464-012-2594-8
Park A, Kavic SM, Lee TH, Heniford BT (2007) Minimally invasive surgery: the evolution of fellowship. Surgery 142:505–513. https://doi.org/10.1016/J.SURG.2007.07.009
Ross SW, Oommen B, Kim M, Walters AL, Green JM, Heniford BT, Augenstein VA (2014) A little slower, but just as good: postgraduate year resident versus attending outcomes in laparoscopic ventral hernia repair. Surg Endosc 28:3092–3100. https://doi.org/10.1007/s00464-014-3586-7
Ross SW, Oommen B, Huntington C, Walters AL, Lincourt AE, Kercher KW, Augenstein VA, Heniford BT (2015) National outcomes for open ventral hernia repair techniques in complex abdominal wall reconstruction. Am Surg 81:778–785
Ross SW, Oommen B, Wormer BA, Walters AL, Matthews BD, Heniford BT, Augenstein VA (2015) National outcomes of laparoscopic Heller myotomy: operative complications and risk factors for adverse events. Surg Endosc 29:3097–3105. https://doi.org/10.1007/s00464-014-4054-0
Ross SW, Seshadri R, Walters AL, Augenstein VA, Heniford BT, Iannitti DA, Martinie JB, Vrochides D, Swan RZ (2016) Mortality in hepatectomy: model for end-stage liver disease as a predictor of death using the National Surgical Quality Improvement Program database. Surgery 159:777–792. https://doi.org/10.1016/j.surg.2015.08.021
American College of Surgeons (2016) ACS National Surgical Quality Improvement Program (ACS NSQIP). https://www.facs.org/quality-programs/acs-nsqip. Accessed 28 Apr 2020
Neuwirth MG, Bartlett EK, Newton AD, Fraker DL, Kelz RR, Roses RE, Karakousis GC (2016) Morbidity and mortality after total splenectomy for lymphoid neoplasms. J Surg Res 205:155–162. https://doi.org/10.1016/j.jss.2016.06.031
Schieman C, Grondin SC (2009) Paraesophageal hernia: clinical presentation, evaluation, and management controversies. Thorac Surg Clin 19:473–484
Richards MK, McAteer JP, Drake FT, Goldin AB, Khandelwal S, Gow KW (2015) A national review of the frequency of minimally invasive surgery among general surgery residents: assessment of ACGME case logs during 2 decades of general surgery resident training. JAMA Surg 150:169–172. https://doi.org/10.1001/jamasurg.2014.1791
Dallemagne B, Kohnen L, Perretta S, Weerts J, Markiewicz S, Jehaes C (2011) Laparoscopic repair of paraesophageal hernia: long-term follow-up reveals good clinical outcome despite high radiological recurrence rate. Ann Surg 253:291–296. https://doi.org/10.1097/SLA.0b013e3181ff44c0
Okrainec A, Ferri LE, Feldman LS, Fried GM (2011) Defining the learning curve in laparoscopic paraesophageal hernia repair: a CUSUM analysis. Surg Endosc 25:1083–1087. https://doi.org/10.1007/s00464-010-1321-6
Udyavar R, Cornwell EE, Havens JM, Hashmi ZG, Scott JW, Sturgeon D, Uribe-Leitz T, Lipsitz SR, Salim A, Haider AH (2018) Surgeon-driven variability in emergency general surgery outcomes: does it matter who is on call? Surgery 164:1109–1116. https://doi.org/10.1016/j.surg.2018.07.008
Helgstrand F, Rosenberg J, Kehlet H, Bisgaard T (2013) Outcomes after emergency versus elective ventral hernia repair: a prospective nationwide study. World J Surg 37:2273–2279. https://doi.org/10.1007/s00268-013-2123-5
Askari A, Malietzis G, Nachiappan S, Antoniou A, Jenkins J, Kennedy R, Faiz O (2015) Defining characteristics of patients with colorectal cancer requiring emergency surgery. Int J Colorectal Dis 30:1329–1336. https://doi.org/10.1007/s00384-015-2313-8
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Sherrill, Rossi, Genz, Matthews, and Reinke have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimer
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Rights and permissions
About this article
Cite this article
Sherrill, W., Rossi, I., Genz, M. et al. Non-elective paraesophageal hernia repair: surgical approaches and short-term outcomes. Surg Endosc 35, 3405–3411 (2021). https://doi.org/10.1007/s00464-020-07782-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07782-3