Abstract
Background
The recent development of 3D vision in laparoscopic and robotic surgical systems raises the question of whether these two procedures are equivalent. The aim of this study was to evaluate the surgical and long-term oncological outcomes of 3D laparoscopic (3D-LLR) and robotic liver resection (RLR) for hepatocellular carcinoma (HCC).
Methods
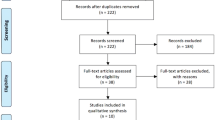
The data for operative time, morbidity, margins, and survival were reviewed for 3D-LLR and compared with RLR.
Results
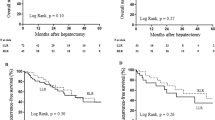
From 2011 to 2017, 93 patients with HCC, including 58 (62%) with cirrhosis, underwent 3D-LLR [49 (53%)] or RLR [44 (47%)]. No difference was observed in operative time (269 vs. 252 min; p = 0.52), overall (27% vs. RLR: 16%; p = 0.49) and severe morbidity (4% vs. 2%; p = 0.77) or in the surgical margin width (9 vs. 11 mm; p = 0.30) between the 3D-LLR and RLR groups. The 3-year overall and recurrence-free survival rates after 3D-LLR and RLR were 82% and 24% and 91% (p = 0.16) and 48% (p = 0.18), respectively.
Conclusions
The 3D-LLR and RLR systems provide comparable surgical margins with similar short- and long-term oncological outcomes.



Similar content being viewed by others
References
EASL Clinical Practice Guidelines (2018) Management of hepatocellular carcinoma. J Hepatol 69(1):182–236
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J (2015) Strasberg SM (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261(4):619–629
Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D'Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS (2009) The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 250(5):825–830
Liu R, Wakabayashi G, Kim HJ, Choi GH, Yiengpruksawan A, Fong Y, He J, Boggi U, Troisi RI, Efanov M, Azoulay D, Panaro F, Pessaux P, Wang XY, Zhu JY, Zhang SG, Sun CD, Wu Z, Tao KS, Yang KH, Fan J, Chen XP (2019) International consensus statement on robotic hepatectomy surgery in 2018. World J Gastroenterol 25(12):1432–1444
Kawai T, Goumard C, Jeune F, Savier E, Vaillant JC, Scatton O (2018) Laparoscopic liver resection for colorectal liver metastasis patients allows patients to start adjuvant chemotherapy without delay: a propensity score analysis. Surg Endosc 32(7):3273–3281
Kawai T, Goumard C, Jeune F, Komatsu S, Soubrane O, Scatton O (2018) 3D vision and maintenance of stable pneumoperitoneum: a new step in the development of laparoscopic right hepatectomy. Surg Endosc 32(8):3706–3712
Lim C, Salloum C, Tudisco A, Ricci C, Osseis M, Napoli N, Lahat E, Boggi U, Azoulay D (2019) Short- and long-term outcomes after robotic and laparoscopic liver resection for malignancies: a propensity score-matched study. World J Surg 43(6):1594–1603
Salloum C, Lim C, Lahat E, Gavara CG, Levesque E, Compagnon P, Azoulay D (2016) Robotic-assisted versus laparoscopic left lateral sectionectomy: analysis of surgical outcomes and costs by a Propensity Score Matched Cohort Study. World J Surg 41(2):516–524
Salloum C, Subar D, Memeo R, Tayar C, Laurent A, Malek A, Azoulay D (2014) Laparoscopic robotic liver surgery: the Henri Mondor initial experience of 20 cases. J Robot Surg 8(2):119–124
Salloum C, Lim C, Azoulay D (2015) Robot-assisted laparoscopic left lateral sectionectomy for benign and malignant liver tumors. J Visc Surg. https://doi.org/10.1016/j.jviscsurg.2015.09.07
Salloum C, Subar D, Memeo R, Tayar C, Laurent A, Malek A, Azoulay D (2013) Laparoscopic robotic liver surgery: the Henri Mondot initial experience of 20 cases. J Robotic Surg. https://doi.org/10.1007/s11701-013-0437-9
Spampinato MG, Coratti A, Bianco L, Caniglia F, Laurenzi A, Puleo F, Ettorre GM, Boggi U (2014) Perioperative outcomes of laparoscopic and robot-assisted major hepatectomies: an Italian multi-institutional comparative study. Surg Endosc 28(10):2973–2979
Boggi U, Caniglia F, Vistoli F, Costa F, Pieroni E, Perrone VG (2015) Laparoscopic robot-assisted resection of tumors located in posterosuperior liver segments. Updates Surg 67(2):177–183
Boggi U, Caniglia F, Amorese G (2013) Laparoscopic robot-assisted major hepatectomy. J Hepatobiliary Pancreat Sci 21(1):3–10
Bismuth H (1982) Surgical anatomy and anatomical surgery of the liver. World J Surg 6(1):3–9
Lim C, Salloum C, Lahat E, Sotirov D, Eshkenazy R, Shwaartz C, Azoulay D (2019) Impact of narrow margin and R1 resection for hepatocellular carcinoma on the salvage liver transplantation strategy. An intention-to-treat analysis. HPB, Oxford
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Büchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149(5):680–688
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan ST, Nimura Y, Figueras J, Capussotti L, Büchler MW, Weitz J (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149(5):713–724
Rahbari NN, Garden OJ, Padbury R, Maddern G, Koch M, Hugh TJ, Fan ST, Nimura Y, Figueras J, Vauthey JN, Rees M, Adam R, Dematteo RP, Greig P, Usatoff V, Banting S, Nagino M, Capussotti L, Yokoyama Y, Brooke-Smith M, Crawford M, Christophi C, Makuuchi M, Büchler MW, Weitz J (2011) Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford) 13(8):528–535
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Slankamenac K, Graf R, Barkun J, Puhan MA, Clavien PA (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258(1):1–7
Benchimol EI, Langan S, Guttmann A (2012) Call to RECORD: the need for complete reporting of research using routinely collected health data. J Clin Epidemiol 66(7):703–705
Famularo S, Giani A, Di Sandro S, Sandini M, Giacomoni A, Pinotti E, Lauterio A, Gianotti L, De Carlis L, Romano F (2017) Does the Pringle maneuver affect survival and recurrence following surgical resection for hepatocellular carcinoma? A western series of 441 patients. J Surg Oncol 117(2):198–206
Xu W, Xu H, Yang H, Liao W, Ge P, Ren J, Sang X, Lu X, Zhong S, Mao Y (2016) Continuous Pringle maneuver does not affect outcomes of patients with hepatocellular carcinoma after curative resection. Asia Pac J Clin Oncol 13(5):e321–e330
Liu S, Li X, Li H, Guo L, Zhang B, Gong Z, Zhang J, Ye Q (2016) Longer duration of the Pringle maneuver is associated with hepatocellular carcinoma recurrence following curative resection. J Surg Oncol 114(1):112–118
Yamashita YI, Hayashi H, Imai K, Okabe H, Nakagawa S, Kitamura F, Uemura N, Nakao Y, Yusa T, Itoyama R, Yamao T, Umesaki N, Miyata T, Chikamoto A, Shimokawa M, Baba H (2019) Perioperative allogeneic blood transfusion does not influence patient survival after hepatectomy for hepatocellular carcinoma: a propensity score matching analysis. World J Surg 43(11):2894–2901
Peng T, Zhao G, Wang L, Wu J, Cui H, Liang Y, Zhou R, Liu Z, Wang Q (2017) No impact of perioperative blood transfusion on prognosis after curative resection for hepatocellular carcinoma: a propensity score matching analysis. Clin Transl Oncol 20(6):719–728
Yang T, Lu JH, Lau WY, Zhang TY, Zhang H, Shen YN, Alshebeeb K, Wu MC, Schwartz M, Shen F (2015) Perioperative blood transfusion does not influence recurrence-free and overall survivals after curative resection for hepatocellular carcinoma: a propensity score matching analysis. J Hepatol 64(3):583–593
Fiorentini G, Swaid F, Cipriani F, Ratti F, Heres C, Tsung A, Aldrighetti L, Geller DA (2019) Propensity score-matched analysis of pure laparoscopic versus hand-assisted/hybrid major hepatectomy at two western centers. World J Surg 43(8):2025–2037
Cho JY, Han HS, Yoon YS, Shin SH (2008) Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 144(1):32–38
Patriti A, Cipriani F, Ratti F, Bartoli A, Ceccarelli G, Casciola L, Aldrighetti L (2014) Robot-assisted versus open liver resection in the right posterior section. JSLS 18(3):e2014
Aghayan DL, Fretland ÅA, Kazaryan AM, Sahakyan MA, Dagenborg VJ, Bjørnbeth BA, Flatmark K, Kristiansen R, Edwin B (2019) Laparoscopic versus open liver resection in the posterosuperior segments: a sub-group analysis from the OSLO-COMET randomized controlled trial. HPB, Oxford
Montalti R, Scuderi V, Patriti A, Vivarelli M, Troisi RI (2015) Robotic versus laparoscopic resections of posterosuperior segments of the liver: a propensity score-matched comparison. Surg Endosc 30(3):1004–1013
Ramanathan R, Salamanca JI, Mandhani A, Leung RA, Rao SR, Berryhill R, Tewari A (2009) Does 3-dimensional (3-D) visualization improve the quality of assistance during robotic radical prostatectomy? World J Urol 27(1):95–99
Funding
The authors do not receive any funding from Intuitive or 3D laparoscopic system.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Chetana Lim, Dr. Claire Goumard, Dr. Chady Salloum, Dr. Antonella Tudisco, Dr. Niccolo Napoli, Prof. Ugo Boggi, Prof. Daniel Azoulay, and Prof. Olivier Scatton have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lim, C., Goumard, C., Salloum, C. et al. Outcomes after 3D laparoscopic and robotic liver resection for hepatocellular carcinoma: a multicenter comparative study. Surg Endosc 35, 3258–3266 (2021). https://doi.org/10.1007/s00464-020-07762-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07762-7