Abstract
Background
Enhanced recovery programs (ERPs), as a rapid rehabilitation method, have been widely used in gastric cancer patients. Although many related studies have confirmed their effectiveness, some patients may still experience poor clinical outcomes. This study analyzed risk factors associated with ERP failure after laparoscopic radical gastrectomy.
Methods
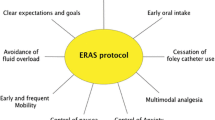
We analyzed the outcomes of 212 patients who underwent ERP following laparoscopic radical gastrectomy between March 2017 and December 2019. The ERP included preoperative education, short periods of fasting, non-mechanical intestinal preparation, early ambulation and oral feeding. ERP failure was defined as more than 7 days of hospitalization due to postoperative complications, unplanned readmission within 30 days of surgery, or death.
Results
The mean patient age was 62 years (range 39–89 years). Surgical procedures included total gastrectomy (n = 161) and distal gastrectomy (n = 51). Overall, 38 (17.9%) patients failed to complete the program, with no mortality. Univariable analysis (P < 0.15) revealed that ERP failure was associated with age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) grade, tumor location, preoperative education, combined operation, long operation time, and significant blood loss. Multivariable analysis (P < 0.05) showed that age, ASA grade III, combined operation and preoperative education were independent risk factors for ERP failure.
Conclusions
We showed that an advanced age, a high ASA grade, lack of a preoperative education and combined surgery were independent risk factors associated with ERP failure after laparoscopic gastrectomy. Therefore, a preoperative patient evaluations and education are important for the success of ERPs.

Similar content being viewed by others
References
Chestovich PJ, Lin AY, Yoo J et al (2013) Fast-track pathways in colorectal surgery. Surg Clin N Am 93:21–32
Wind J, Hofland J, Bemelman WA et al (2006) Perioperative strategy in colonic surgery; LAparoscopy and/or FAst track multimodal management versus standard care (LAFA trial). BMC Surg 6:16
Soop M, Carlson GL, Ljungqvist O et al (2004) Randomized clinical trial of the effects of immediate enteral nutrition on metabolic responses to major colorectal surgery in an enhanced recovery protocol. Br J Surg 91:1138–1145
Lee TG, Kang SB, Park KJ et al (2011) Comparison of early mobilization and diet rehabilitation program with conventional care after laparoscopic colon surgery: a prospective randomized controlled trial. Dis Colon Rectum 54:21–28
Vlug MS, Wind J, Group LS et al (2011) Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: a randomized clinical trial (LAFA-study). Ann Surg 254:868–875
Zhuang CL, Ye XZ, Yu Z et al (2013) Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum 56:667–678
Wilmore DW, Kehlet H (2001) Management of patients in fast track surgery. BMJ 322:473–476
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 248:189–198
Nicholson A, Lowe MC, Smith AF (2014) Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg 101:172–188
Varadhan KK, Neal KR, Dong CH et al (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta analysis of randomized controlled trials. Clin Nutr 29(4):434–440
Robotic and Laparoscopic Surgery Committee of Chinese Research Hospital Association (2017) Expert consensus on enhanced recovery after gastrectomy for gastric cancer (2016 edition). Chin J Dig Surg 1(1):16
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240:205–213
Aarts MA, Okrainec A, McLeod RS et al (2012) Adoption of enhanced recovery after surgery (ERAS) strategies for colorectal surgery at academic teaching hospitals and impact on total length of hospital stay. Surg Endosc 26:442–450
Kehlet H (2015) Enhanced Recovery After Surgery (ERAS): good for now, but what about the future? Can J Anaesth 62(2):99–104
Pearsall EA, Meghji Z, Pitzul KB (2015) A qualitative study to understand the barriers and enablers in implementing an enhanced recovery after surgery program. Ann Surg 261(1):92–96
Kulaylat AN, Dillon PW, Stewart DB et al (2015) Determinants of 30-d readmission after colectomy. J Surg Res 193:528–535
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Chenxing Jian, Jianying Fang, Limin Wu, Zifang Zheng, Yucheng Song, Wei Liu, Xiaoning Lin, and Chunkang Yang have no potential conflicts of interest to disclose.
Ethical approval
The Institutional Review Board of the Affiliated Hospital of Putian University approved this study prior to the commencement of data collection and analysis (No: 201808).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jian, C., Fang, J., Wu, L. et al. Failure of enhanced recovery programs after laparoscopic radical gastrectomy: a single-center retrospective study. Surg Endosc 35, 2629–2635 (2021). https://doi.org/10.1007/s00464-020-07683-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07683-5