Abstract
Background
Videoscopic inguinal lymphadenectomy (VIL) represents an innovative approach for patients with melanoma lymph node (LN) metastases, mainly aimed at lowering wound-related morbidity. However, long-term data on oncologic safety are still lacking. The aim of this study is to review the oncologic outcome of videoscopic groin dissection in a single institution caseload.
Methods
Data were prospectively gathered on patients with inguinal melanoma metastasis who underwent VIL. Clinical data included age, race, sex, tumor histology, node counts and number of metastatic nodes. Disease-free survival and overall survival were monitored based on an institutional follow-up schedule. The study was approved by the local ethics committee (Video-SIIO II study).
Results
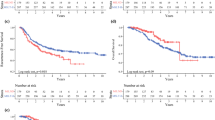
We analyzed 48 videoscopic groin dissections performed in 50 patients (2 patients underwent bilateral VIL). Median age was 54.5 years. Female/male ratio was 15/33. Indication for surgery was positive inguinal sentinel biopsy and cytological confirmed clinical disease in 40 and 10 cases, respectively. Median LN retrieval count was 19. After a median follow-up of 28 months, groin recurrence (lymphatic basin) was observed in one single case.
Conclusions
VIL for melanoma LN metastases is associated with a favorable oncologic outcome. In particular, LN yield and locoregional recurrence rate obtained with videoscopic dissection are comparable to those reported with the open technique. Prospective studies are needed to confirm these results in a larger cohort of patients.

Similar content being viewed by others
References
Gershenwald JE, Scolyer RA, Hess KR, Sondak VK, Long GV, Ross MI, Lazar AJ, Faries MB, Kirkwood JM, Mcarthur GA, Haydu LE, Eggermont AMM, Flaherty KT, Balch CM, Thompson JF, for members of the American Joint Committee on Cancer Melanoma Expert Panel and the International Melanoma Database and Discovery Platform (2017) Melanoma staging: evidence-based changes in the American Joint Committee on Cancer Eighth Edition Cancer Staging Manual. Cancer J Clin 67:472–492
Wong SL, Faries MB, Kennedy EB, Agarwala SS, Akhurst TJ, Ariyan C, Balch CM, Berman BS, Cochran A, Delman KA, Gorman M, Kirkwood JM, Moncrieff MD, Zager JS, Lyman GH (2018) Sentinel lymph node biopsy and management of regional lymph nodes in melanoma: American Society of Clinical Oncology and Society of Surgical Oncology Clinical Practice Guideline Update. J Clin Oncol 36:399–413
Leiter U, Stadler R, Mauch C, Hohenberger W, Brockmeyer N, Berking C, Sunderkötter C, Kaatz M, Schulte KW, Lehmann P, Vogt T, Ulrich J, Herbst R, Gehring W, Simon JC, Keim U, Martus P, Garbe C, German Dermatologic Cooperative Oncology Group (DeCOG) (2016) Complete lymph node dissection versus no dissection in patients with sentinel lymph node biopsy positive melanoma (DeCOG-SLT): a multicenter, randomized, phase 3 trial. Lancet Oncol 17:757–767
Faries MB, Thompson JF, Cochran AJ, Andtbacka RH, Mozzillo N, Zager JS, Jahkola T, Bowles TL, Testori A, Beitsch PD, Hoekstra HJ, Moncrieff M, Ingvar C, Wouters MWJM, Sabel MS, Levine EA, Agnese D, Henderson M, Dummer R, Rossi CR, Neves RI, Trocha SD, Wright F, Byrd DR, Matter M, Hsueh E, MacKenzie-Ross A, Johnson DB, Terheyden P, Berger AC, Huston TL, Wayne JD, Smithers BM, Neuman HB, Schneebaum S, Gershenwald JE, Ariyan CE, Desai DC, Jacobs L, McMasters KM, Gesierich A, Hersey P, Bines SD, Kane JM, Barth RJ, McKinnon G, Farma JM, Schultz E, Vidal-Sicart S, Hoefer RA, Lewis JM, Scheri R, Kelley MC, Nieweg OE, Noyes RD, Hoon DSB, Wang HJ, Elashoff DA, Elashoff RM (2017) Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med 376:2211–2222
de Vries M, Vonkeman WG, van Ginkel RJ, Hoekstra HJ (2006) Morbidity after inguinal sentinel lymph node biopsy and completion lymph node dissection in patients with cutaneous melanoma. Eur J Surg Oncol 32:785–789
Chang SB, Askew RL, Xing Y, Weaver S, Gershenwald JE, Lee JE, Royal R, Lucci A, Ross MI, Cormier JN (2010) Prospective assessment of postoperative complications and associated costs following inguinal lymph node dissection in melanoma patients. Ann Surg Oncol 17:2764–2772
Stuiver MM, Westerduin E, ter Meulen S, Vincent AD, Nieweg OE, Wouters MW (2014) Surgical wound complications after groin dissection in melanoma patients—a historical cohort study and risk factor analysis. Eur J Surg Oncol 40:1284–1290
Sommariva A (2018) Other approach for reducing surgical risk. In: Delamn KA, Master VA (eds) Malignancies of the groin, surgical and anatomic considerations. Springer, New York, pp 207–221
Moody JA, Botham SJ, Dahill KE, Wallace DL, Hardwicke JT (2017) Complications following completion lymphadenectomy versus therapeutic lymphadenectomy for melanoma—a systematic review of the literature. Eur J Surg Oncol 43:1760–1767
Bilimoria KY, Balch CM, Bentrem DJ, Talamonti MS, Ko CY, Lange JR, Winchester DP, Wayne JD (2008) Complete lymph node dissection for sentinel node-positive melanoma: assessment of practice patterns in the United States. Ann Surg Oncol 15:1566–1576
Sommariva A, Pasquali S, Rossi CR (2015) Video endoscopic inguinal lymphadenectomy for lymph node metastasis from solid tumors. Eur J Surg Oncol 41:274–281
Delman KA, Kooby DA, Ogan K, Hsiao W, Master V (2010) Feasability of novel approach to inguinal lymphadenectomy: minimally invasive groin dissection for melanoma. Ann Surg Oncol 17:731–737
Abbott AM, Grotz TE, Rueth NM, Hernandez Irizarry RC, Tuttle TM, Jakub JW (2013) Minimally invasive inguinal lymph node dissection (MILND) for melanoma: experience from two academic centers. Ann Surg Oncol 20:340–345
Sommariva A, Pasquali S, Cona C, Ciccarese AA, Saadeh L, Campana LG, Meroni M, Rossi CR (2016) Videoscopic ilioinguinal lymphadenectomy for groin lymph node metastases from melanoma. Br J Surg 103:1026–1032
Vrielink OM, Faut M, Deckers EA, van Leeuwen BL, Been LB (2019) Evaluation of the videoscopic inguinal lymphadenectomy in melanoma patients. Eur J Surg Oncol 45:1712–1716
Martin BM, Etra JW, Russell MC, Rizzo M, Kooby DA, Staley CA, Master VA, Delman KA (2014) Oncologic outcomes of patients undergoing videoscopic inguinal lymphadenectomy for metastatic melanoma. J Am Coll Surg 218:620–626
General Assembly of the World Medical Association World Medical Association (2014) Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent 81:14–18
Charlson ME, Charlson RE, Peterson JC, Marinopoulos SS, Briggs WM, Hollenberg JP (2008) The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. J Clin Epidemiol 61:1234–1240
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-years experience. Ann Surg 250:187–196
Jakub JW, Terando AM, Sarnaik A, Ariyan CE, Faries MB, Zani Jr S, Neuman HB, Wasif N, Farma JM, Averbook BJ, Bilimoria KY, Grotz TE, Allred JB, Suman VJ, Brady MS, Tyler D, Wayne JD, Nelson H, Sarnaik A (2017) Safety and feasibility of minimally invasive inguinal lymph node dissection in patients with melanoma (SAFE-MILND): report of a prospective multi-institutional trial. Ann Surg 265:192–196
Zendejas B, Jakub JW, Terando AM, Sarnaik A, Ariyan CE, Faries MB, Zani Jr S, Neuman HB, Wasif N, Farma JM, Averbook BJ, Bilimoria KY, Tyler D, Brady MS, Farley DR (2017) Laparoscopic skill assessment of practicing surgeons prior to enrollment in a surgical trial of a new laparoscopic procedure. Surg Endosc 31:3313–3319
Pasquali S, Sommariva A, Spillane AJ, Bilimoria KY, Rossi CR (2017) Measuring the quality of melanoma surgery: highlighting issues with standardization and quality assurance of care in surgical oncology. Eur J Surg Oncol 43:561–571
Spillane AJ, Haydu L, McMillan W, Stretch JR, Thompson JF (2011) Quality assurance parameters and predictors of outcome for ilioinguinal and inguinal dissection in a contemporary melanoma patient population. Ann Surg Oncol 18:2521–2528
Rossi CR, Mozzillo N, Maurichi A, Pasquali S, Macripò G, Borgognoni L, Solari N, Piazzalunga D, Mascheroni L, Giudice G, Mocellin S, Patuzzo R, Caracò C, Ribero S, Marone U, Santinami M (2014) Number of excised lymph nodes as a quality assurance measure for lymphadenectomy in melanoma. JAMA Surg 149:700–706
Postlewait LM, Farley CR, Diller ML, Martin B, Hart Squires III M, Russell MC, Rizzo M, Ogan K, Master V, Delman K (2017) A minimally invasive approach for inguinal lymphadenectomy in melanoma and genitourinary malignancy: long-term outcomes in an attempted randomized control trial. Ann Surg Oncol 24:3237–3244
Acknowledgments
The authors wish to thank Ms. Christina Drace for English editing.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Antonio Sommariva, Camilla Cona, Marco Tonello, Pierluigi Pilati and Carlo Riccardo Rossi have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sommariva, A., Cona, C., Tonello, M. et al. Oncological outcome of videoscopic groin dissection for lymph node metastasis from melanoma. Surg Endosc 35, 2576–2582 (2021). https://doi.org/10.1007/s00464-020-07675-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07675-5