Abstract
Objective
Indeterminate biliary strictures remain a significant diagnostic challenge. Digital single-operator cholangioscopy (D-SOC) incorporates digital imaging which enables higher resolution for better visualization and diagnosis of biliary pathology. We aimed to conduct a systematic review and meta-analysis of available literature in an attempt to determine the efficacy of D-SOC in the visual interpretation of indeterminate biliary strictures.
Material and methods
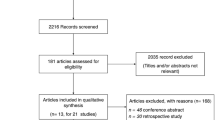
Electronic searches were performed using Medline (PubMed), EMBASE, and Cochrane Library. All D-SOC studies that reported the diagnostic performance in visual interpretation of indeterminate biliary strictures and biliary malignancies were included. The Quality Assessment of Diagnostic Accuracy Studies (QUADAS)-2 was used to evaluate the quality of the included studies. All data were extracted and pooled to construct a 2 × 2 table. The visual interpretation of D-SOC was compared to resected surgical specimens or clinical follow-up in the included patients. Pooled sensitivity, specificity, positive predictive value, negative predictive value, prevalence, positive likelihood ratio (+LR), negative likelihood ratio (−LR), and diagnostic odds ratio (OR) were calculated. The summarized receiver operating characteristic (SROC) curve corresponding with the area under the curve (AUC) was also analyzed.
Results
The search yielded 465 citations. Of these, only six studies with a total of 283 procedures met inclusion criteria and were included in the meta-analysis. The overall pooled sensitivity and specificity of D-SOC in the visual interpretation of biliary malignancies was 94% (95% CI 89–97) and 95% (95%CI 90–98), respectively, while +LR, −LR, diagnostic OR, and AUC were 15.20 (95%CI 5.21–44.33), 0.08 (95%CI 0.04–0.14), 308.83 (95%CI 106.46–872.82), and 0.983, respectively. The heterogeneity among 6 included studies was moderate for specificity (I2 = 0.51) and low for sensitivity (I2 = 0.17) and diagnostic OR (I2 = 0.00).
Conclusion
D-SOC is associated with high sensitivity and specificity in the visual interpretation of indeterminate biliary strictures and malignancies. D-SOC should be considered routinely in the diagnostic workup of indeterminate biliary lesions.




Similar content being viewed by others
References
Nakajima M, Akasaka Y, Yamaguchi K, Fujimoto S, Kawai K (1978) Direct endoscopic visualization of the bile and pancreatic duct systems by peroral cholangiopancreatoscopy (PCPS). Gastrointest Endosc 24:141–145. https://doi.org/10.1016/S0016-5107(78)73488-7
Ishida Y, Itoi T, Okabe Y (2019) Current status and future perspective in cholangiopancreatoscopy. Curr Treat Opt Gastroenterol 17:327–341. https://doi.org/10.1007/s11938-019-00238-1
Parsa N, Khashab MA (2019) The role of peroral cholangioscopy in evaluating indeterminate biliary strictures. Clin Endosc 52:556–564. https://doi.org/10.5946/ce.2019.011
Franzini T, Moura R, Bonifácio P, Luz G, de Souza T, dos Santos M, Rodela G, Ide E, Herman P, Montagnini A, D’Albuquerque L, Sakai P, de Moura E (2018) Complex biliary stones management: cholangioscopy versus papillary large balloon dilation—a randomized controlled trial. Endosc Int Open 06:E131–E138. https://doi.org/10.1055/s-0043-122493
Bang JY, Navaneethan U, Hasan M, Sutton B, Hawes R, Varadarajulu S (2020) Optimizing outcomes of single-operator cholangioscopy-guided biopsies based on a randomized trial. Clin Gastroenterol Hepatol 18:441–448.e1. https://doi.org/10.1016/j.cgh.2019.07.035
De Moura DTH, Coronel M, Ribeiro IB, Farias GFA, Choez MA, Rocha R, Toscano MP, De Moura EGH (2018) The importance of endoscopic ultrasound fine-needle aspiration in the diagnosis of solid pseudopapillary tumor of the pancreas: two case reports. J Med Case Rep 12:107. https://doi.org/10.1186/s13256-018-1585-3
Franzini TAP, Moura RN, de Moura EGH (2016) Advances in therapeutic cholangioscopy. Gastroenterol Res Pract 2016:1–7. https://doi.org/10.1155/2016/5249152
Franzini T, Sagae VMT, Guedes HG, Sakai P, Waisberg DR, Andraus W, D’Albuquerque LAC, Sethi A, de Moura EGH (2019) Cholangioscopy-guided steroid injection for refractory post liver transplant anastomotic strictures: a rescue case series. Ther Adv Gastrointest Endosc 12:263177451986778. https://doi.org/10.1177/2631774519867786
de Rocha RSP, Minata MK, de Moura DTH, de Moura EGH, Franzini TAP (2018) Common bile duct intussusception during ERCP for stone removal. VideoGIE 3:28–30. https://doi.org/10.1016/j.vgie.2017.09.003
Franzini T, Cardarelli-Leite L, Figueira E, Morita F, Domingos F, Carnevale F, de Moura E (2017) SpyGlass percutaneous transhepatic cholangioscopy-guided lithotripsy of a large intrahepatic stone. Endoscopy 49:E292–E293. https://doi.org/10.1055/s-0043-117943
Pereira P, Santos S, Morais R, Gaspar R, Rodrigues-Pinto E, Vilas-Boas F, Macedo G (2020) Role of peroral cholangioscopy for diagnosis and staging of biliary tumors. Dig Dis. https://doi.org/10.1159/000504910
Gerges C, Beyna T, Tang RSY, Bahin F, Lau JYW, van Geenen E, Neuhaus H, Reddy DN, Ramchandani M (2019) Digital single-operator peroral cholangioscopy-guided biopsy versus ERCP-guided brushing for indeterminate biliary strictures: a prospective, randomized multicenter trial (with video). Gastrointest Endosc. https://doi.org/10.1016/j.gie.2019.11.025
de Moura DTH, Ryou M, de Moura EGH, Ribeiro IB, Bernardo WM, Thompson CC (2019) EUS-guided fine needle aspiration and ERCP-based tissue sampling in suspected malignant biliary strictures: a meta-analysis of same-session procedures. Clin Endosc. https://doi.org/10.5946/ce.2019.053
Passos ML, Ribeiro IB, de Moura DTH, Korkischko N, Silva GLR, Franzini TP, Bernando WM, de Moura EGH (2019) Efficacy and safety of carbon dioxide insufflation versus air insufflation during endoscopic retrograde cholangiopancreatography in randomized controlled trials: a systematic review and meta-analysis. Endosc Int open 7:E487–E497. https://doi.org/10.1055/a-0854-3739
Serrano JPR, de Moura DTH, Bernardo WM, Ribeiro IB, Franzini TP, de Moura ETH, Brunaldi VO, Salesse MT, Sakai P, De Moura EGH (2019) Nonsteroidal anti-inflammatory drugs versus placebo for post-endoscopic retrograde cholangiopancreatography pancreatitis: a systematic review and meta-analysis. Endosc Int open 7:E477–E486. https://doi.org/10.1055/a-0862-0215
Visconti T, Bernardo W, Moura D, Moura E, Gonçalves C, Farias G, Guedes H, Ribeiro I, Franzini T, Luz G, dos Santos M, de Moura E (2018) Metallic vs plastic stents to treat biliary stricture after liver transplantation: a systematic review and meta-analysis based on randomized trials. Endosc Int Open 06:E914–E923. https://doi.org/10.1055/a-0626-7048
de Delgado AAA, de Moura DTH, Ribeiro IB, Bazarbashi AN, dos Santos MEL, Bernardo WM, de Moura EGH (2019) Propofol vs traditional sedatives for sedation in endoscopy: a systematic review and meta-analysis. World J Gastrointest Endosc 11:573–588. https://doi.org/10.4253/wjge.v11.i12.573
Matsubayashi CO, Ribeiro IB, de Moura DTH, Brunaldi VO, Bernardo WM, Hathorn KE, de Moura EGH (2020) Is endoscopic balloon dilation still associated with higher rates of pancreatitis?: A systematic review and meta-analysis. Pancreas 49:158–174. https://doi.org/10.1097/MPA.0000000000001489
Funari MP, Ribeiro IB, de Moura DTH, Bernardo WM, Brunaldi VO, Rezende DT, Resende RH, de Marco MO, Franzini TAP, de Moura EGH (2020) Adverse events after biliary sphincterotomy: Does the electric current mode make a difference? A systematic review and meta-analysis of randomized controlled trials. Clin Res Hepatol Gastroenterol. https://doi.org/10.1016/j.clinre.2019.12.009
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Leeflang MM, Deeks JJ, Takwoingi Y, Macaskill P (2013) Cochrane diagnostic test accuracy reviews. Syst Rev 2:82. https://doi.org/10.1186/2046-4053-2-82
Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MMG, Sterne JAC, Bossuyt PMM, QUADAS-2 Group (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Analysis of Binary Data. In: The Concise Encyclopedia of Statistics. Springer New York, New York, NY, pp 4–5
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31. https://doi.org/10.1186/1471-2288-6-31
Shah R, Raijman I, Brauer B, Gumustop B, Pleskow D (2017) Performance of a fully disposable, digital, single-operator cholangiopancreatoscope. Endoscopy 49:651–658. https://doi.org/10.1055/s-0043-106295
Ang T, Kwek A (2019) Safety and efficacy of SpyGlass cholangiopancreatoscopy in routine clinical practice in a regional Singapore hospital. Singapore Med J 60:538–544. https://doi.org/10.11622/smedj.2018158
Urban O, Evinová E, Fojtík P, Loveček M, Kliment M, Zoundjiekpon V, Falt P (2018) Digital cholangioscopy: the diagnostic yield and impact on management of patients with biliary stricture. Scand J Gastroenterol 53:1364–1367. https://doi.org/10.1080/00365521.2018.1512649
Lenze F, Bokemeyer A, Gross D, Nowacki T, Bettenworth D, Ullerich H (2018) Safety, diagnostic accuracy and therapeutic efficacy of digital single-operator cholangioscopy. United Eur Gastroenterol J 6:902–909. https://doi.org/10.1177/2050640618764943
Turowski F, Hügle U, Dormann A, Bechtler M, Jakobs R, Gottschalk U, Nötzel E, Hartmann D, Lorenz A, Kolligs F, Veltzke-Schlieker W, Adler A, Becker O, Wiedenmann B, Bürgel N, Tröger H, Schumann M, Daum S, Siegmund B, Bojarski C (2018) Diagnostic and therapeutic single-operator cholangiopancreatoscopy with SpyGlassDSTM: results of a multicenter retrospective cohort study. Surg Endosc 32:3981–3988. https://doi.org/10.1007/s00464-018-6141-0
Yan S, Tejaswi S (2019) Clinical impact of digital cholangioscopy in management of indeterminate biliary strictures and complex biliary stones: a single-center study. Ther Adv Gastrointest Endosc 12:263177451985316. https://doi.org/10.1177/2631774519853160
Kim H-J, Kim M-H, Lee S-K, Yoo K-S, Seo D-W, Min Y-I (2000) Tumor vessel: A valuable cholangioscopic clue of malignant biliary stricture. Gastrointest Endosc 52:635–638. https://doi.org/10.1067/mge.2000.108969
Fukuda Y, Tsuyuguchi T, Sakai Y, Tsuchiya S, Saisyo H (2005) Diagnostic utility of peroral cholangioscopy for various bile-duct lesions. Gastrointest Endosc 62:374–382. https://doi.org/10.1016/j.gie.2005.04.032
Robles-Medranda C, Valero M, Soria-Alcivar M, Puga-Tejada M, Oleas R, Ospina-Arboleda J, Alvarado-Escobar H, Baquerizo-Burgos J, Robles-Jara C, Pitanga-Lukashok H (2018) Reliability and accuracy of a novel classification system using peroral cholangioscopy for the diagnosis of bile duct lesions. Endoscopy 50:1059–1070. https://doi.org/10.1055/a-0607-2534
Badshah MB, Vanar V, Kandula M, Kalva N, Badshah MB, Revenur V, Bechtold ML, Forcione DG, Donthireddy K, Puli SR (2019) Peroral cholangioscopy with cholangioscopy-directed biopsies in the diagnosis of biliary malignancies. Eur J Gastroenterol Hepatol 31:935–940. https://doi.org/10.1097/MEG.0000000000001402
Sun X, Zhou Z, Tian J, Wang Z, Huang Q, Fan K, Mao Y, Sun G, Yang Y (2015) Is single-operator peroral cholangioscopy a useful tool for the diagnosis of indeterminate biliary lesion? A systematic review and meta-analysis. Gastrointest Endosc 82:79–87. https://doi.org/10.1016/j.gie.2014.12.021
Moura D, de Moura E, Matuguma S, dos Santos M, Moura E, Baracat F, Artifon E, Cheng S, Bernardo W, Chacon D, Tanigawa R, Jukemura J (2018) EUS-FNA versus ERCP for tissue diagnosis of suspect malignant biliary strictures: a prospective comparative study. Endosc Int Open 06:E769–E777. https://doi.org/10.1055/s-0043-123186
De Moura DH, De MEH, Bernardo W, De Moura EH, Baraca F, Kondo A, Matuguma S, Almeida Artifon E (2018) Endoscopic retrograde cholangiopancreatography versus endoscopic ultrasound for tissue diagnosis of malignant biliary stricture: systematic review and meta-analysis. Endosc Ultrasound 7:10. https://doi.org/10.4103/2303-9027.193597
Navaneethan U, Hasan MK, Lourdusamy V, Njei B, Varadarajulu S, Hawes RH (2015) Single-operator cholangioscopy and targeted biopsies in the diagnosis of indeterminate biliary strictures: a systematic review. Gastrointest Endosc 82:608–614.e2. https://doi.org/10.1016/j.gie.2015.04.030
Funding
None.
Author information
Authors and Affiliations
Contributions
PVAGO: acquisition of data, analysis, interpretation of data, drafting the article, revising the article, final approval; DTHDM: acquisition of data, analysis, interpretation of data, drafting the article, revising the article, final approval; IBR: analysis and interpretation of data, revising the article; ANDB: analysis and interpretation of data, revising the article; TPF: analysis and interpretation of data, drafting the article, final approval; MELDS: analysis and interpretation of data, drafting the article, final approval; WMB: analysis and interpretation of data, drafting the article, final approval; EGHDM analysis and interpretation of data, drafting the article, revising the article, final approval;
Corresponding author
Ethics declarations
Disclosures
Drs. Tomazo Antonio Prince Franzin and Marcos Eduardo Lera dos Santos reports personal fees from BOSTON SCIENTIFIC, outside the submitted work; Dr. Eduardo Guimarães Hourneaux de Moura reports personal fees from Boston Scientific, personal fees from Olympus, outside the submitted work. Drs. Pedro Victor Aniz Gomes de Oliveira, Diogo Turiani Hourneaux de Moura, Igor Braga Ribeiro, Ahmad Najdat Bazarbashi, and Wanderley Marques Bernardo have nothing to disclose.
Ethical approval
The study was approved by the Research Ethics Committee of the University of São Paulo School of Medicine Hospital das Clínicas and written consent was not required as this was a systematic review project.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Oliveira, P.V.A.G., de Moura, D.T.H., Ribeiro, I.B. et al. Efficacy of digital single-operator cholangioscopy in the visual interpretation of indeterminate biliary strictures: a systematic review and meta-analysis. Surg Endosc 34, 3321–3329 (2020). https://doi.org/10.1007/s00464-020-07583-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07583-8