Abstract
Background
Although postoperative strictures after endoscopic submucosal dissection (ESD) in the rectum are relatively rare, some rectal lesions require resection involving the anal canal, which is a narrow tract comprising squamous epithelium. To the best of our knowledge, no studies have investigated narrow anal canals when evaluating post-ESD strictures. This study aimed to evaluate the impact of resections involving the anal canal on postoperative stricture development.
Methods
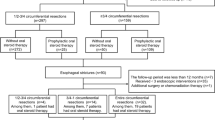
Between April 2005 and October 2017, 707 rectal lesions were treated with ESD. We retrospectively investigated 102 lesions that required ≥ 75% circumferential resection. Risk factors for post-ESD stricture and, among patients with strictures, obstructive symptoms, and number of dilation therapies required were investigated.
Results
Post-ESD stricture occurred in 18 of 102 patients (17.6%). In the multivariate analysis, circumferential resection ≥ 90% and ESD involving the anal canal (ESD-IAC) were risk factors for postoperative strictures (P ≤ 0.0001 and 0.0115, respectively). Among the patients with strictures, obstructive symptoms were significantly related to anal strictures compared to rectal strictures (100% vs. 27.2%, P = 0.0041). Furthermore, the number of dilation therapies required was significantly greater among patients with anal strictures compared to those with rectal strictures (6.5 times vs. 2.7 times, P = 0.0263).
Conclusion
Not only circumferential resection ≥ 90% but also ESD-IAC was a significant risk factor for the stricture after rectal ESD. Furthermore, anal strictures were associated with a significantly higher frequency of obstructive symptoms and larger number of required dilation therapies than were rectal strictures.




Similar content being viewed by others
References
Saito Y, Uraoka T, Yamaguchi Y et al (2010) A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 72:1217–1225
Fujishiro M, Yahagi N, Kakushima N et al (2007) Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol 5:678–683
Tamegai Y, Saito Y, Masaki N et al (2007) Endoscopic submucosal dissection: a safe technique for colorectal tumors. Endoscopy 39:418–422
Niimi K, Fujishiro M, Kodashima S et al (2010) Long-term outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy 42:723–729
Kiriyama S, Saito Y, Yamamoto S et al (2012) Comparison of endoscopic submucosal dissection with laparoscopic-assisted colorectal surgery for early-stage colorectal cancer: a retrospective analysis. Endoscopy 44:1024–1030
Toyonaga T, Man-i M, East JE et al (2013) 1,635 Endoscopic submucosal dissection cases in the esophagus, stomach, and colorectum: complication rates and long-term outcomes. Surg Endosc 27:1000–1008
Ohata K, Nonaka K, Minato Y et al (2013) Endoscopic submucosal dissection for large colorectal tumor in a Japanese General Hospital. J Oncol 2013:1–4
Lee EJ, Lee JB, Lee SH et al (2013) Endoscopic submucosal dissection for colorectal tumors-1,000 colorectal ESD cases: one specialized institute's experiences. Surg Endosc 27:31–39
Nakajima T, Saito Y, Tanaka S et al (2013) Current status of endoscopic resection strategy for large, early colorectal neoplasia in Japan. Surg Endosc 27:3262–3270
Oka S, Tanaka S, Saito Y et al (2015) Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol 110:697–707
Antillon MR, Bartalos CR, Miller ML et al (2008) En bloc endoscopic submucosal dissection of a 14-cm laterally spreading adenoma of the rectum with involvement to the anal canal: expanding the frontiers of endoscopic surgery (with video). Gastrointest Endosc 67:332–337
Ohara Y, Toyonaga T, Tsubouchi E et al (2016) Clinical course after endoscopic submucosal dissection in the rectum leaving a circumferential mucosal defect of 26 cm in length. Endoscopy 48:E4–E5
Hayashi Y, Shinozaki S, Sunada K et al (2016) Efficacy and safety of endoscopic submucosal dissection for superficial colorectal tumors more than 50 mm in diameter. Gastrointest Endosc 83:602–607
Ohara Y, Toyonaga T, Tanaka S et al (2015) Risk of stricture after endoscopic submucosal dissection for large rectal neoplasms. Endoscopy 48:62–70
Abe S, Sakamoto T, Takamaru H et al (2016) Stenosis rates after endoscopic submucosal dissection of large rectal tumors involving greater than three quarters of the luminal circumference. Surg Endosc 30:5459–5464
Hayashi T, Kudo SE, Miyachi H et al (2017) Management and risk factor of stenosis after endoscopic submucosal dissection for colorectal neoplasms. Gastrointest Endosc 86:358–369
Nakadoi K, Tanaka S, Hayashi N et al (2012) Clinical outcomes of endoscopic submucosal dissection for rectal tumor close to the dentate line. Gastrointest Endosc 76:444–450
Imai K, Hotta K, Yamaguchi Y et al (2015) Safety and efficacy of endoscopic submucosal dissection of rectal tumors extending to the dentate line. Endoscopy 47:529–532
Tamaru Y, Oka S, Tanaka S et al (2016) Endoscopic submucosal dissection for anorectal tumor with hemorrhoids close to the dentate line: a multicenter study of Hiroshima GI Endoscopy Study Group. Surg Endosc 30:4425–4431
Tanaka S, Toyonaga T, Morita Y et al (2016) Feasibility and safety of endoscopic submucosal dissection for lower rectal tumors with hemorrhoids. World J Gastroenterol 22:6268–6275
Matsumoto S, Mashima H (2017) The efficacy of endoscopic submucosal dissection for colorectal tumors extending to the dentate line. Int J Colorectal Dis 32:831–837
Ono S, Fujishiro M, Niimi K et al (2009) Predictors of postoperative stricture after esophageal endoscopic submucosal dissection for superficial squamous cell neoplasms. Endoscopy 41:661–665
Shi Q, Ju H, Yao LQ et al (2014) Risk factors for postoperative stricture after endoscopic submucosal dissection for superficial esophageal carcinoma. Endoscopy 46:640–644
Coda S, Oda I, Gotoda T et al (2009) Risk factors for cardiac and pyloric stenosis after endoscopic submucosal dissection, and efficacy of endoscopic balloon dilation treatment. Endoscopy 41:421–426
Iizuka H, Kakizaki S, Sohara N et al (2010) Stricture after endoscopic submucosal dissection for early gastric cancers and adenomas. Dig Endosc 22:282–288
Tanaka S, Kashida H, Saito Y et al (2015) JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc 27:417–434
Saito Y, Uraoka T, Matsuda T et al (2007) A pilot study to assess the safety and efficacy of carbon dioxide insufflation during colorectal endoscopic submucosal dissection with the patient under conscious sedation. Gastrointest Endosc 65:537–542
Fujishiro M, Yahagi N, Kashimura K et al (2004) Comparison of various submucosal injection solutions for maintaining mucosal elevation during endoscopic mucosal resection. Endoscopy 36:579–583
Toyonaga T, Man IM, Fujita T et al (2010) The performance of a novel ball-tipped Flush knife for endoscopic submucosal dissection: a case-control study. Aliment Pharmacol Ther 32:908–915
Takeuchi Y, Uedo N, Ishihara R et al (2010) Efficacy of an endo-knife with a water-jet function (Flushknife) for endoscopic submucosal dissection of superficial colorectal neoplasms. Am J Gastroenterol 105:314–322
Ohara Y, Toyonaga T, Hoshi N et al (2017) Usefulness of a novel slim type FlushKnife-BT over conventional FlushKnife-BT in esophageal endoscopic submucosal dissection. World J Gastroenterol 23:1657–1665
Watanabe T, Itabashi M, Shimada Y et al (2012) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol 17:1–29
Tsuda M, Ohnishi S, Mizushima T et al (2018) Preventive effect of mesenchymal stem cell culture supernatant on luminal stricture after endoscopic submucosal dissection in the rectum of pigs. Endoscopy 50:1001–1016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Tomoya Sako, Takashi Toyonaga, Yoshiko Nakano, Shinwa Tanaka, Toshitatsu Takao, Shinichi Baba, Hiroshi Takihara, Yoshinori Morita, Eiji Umegaki, and Yuzo Kodama have no conflicts of interest or financial ties to disclose.
Informed consent
Written informed consent was obtained from all participants before the ESD procedures and the study design was approved by the ethics committee at Kobe University Hospital and Kishiwada Tokushukai Hospital (180147). The study was conducted in accordance with principles of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sako, T., Toyonaga, T., Nakano, Y. et al. Endoscopic submucosal dissection involving the anal canal presents a risk factor for postoperative stricture. Surg Endosc 35, 1307–1316 (2021). https://doi.org/10.1007/s00464-020-07508-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07508-5