Abstract
Background
Operating room (OR) efficiency requires coordinated teamwork between the staff surgeon, anesthesia team, circulating nurse, surgical technician, and surgical trainee or assistant. Bariatric cases present unique challenges including difficult airways, challenging intravenous access, use of specialized surgical equipment, and synchronized exchange of orogastric tubes. The high contribution margin of these complex bariatric procedures rests on OR efficiency.
Objective
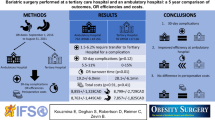
To compare the efficiency of bariatric surgeries performed by a single surgeon at a tertiary academic medical center with its inherent variability of OR staff to that of a private hospital with a standardized surgical team.
Methods
All laparoscopic Roux-en-Y gastric bypasses (LRYGB) performed by a single surgeon at University Hospitals Cleveland Medical Center (UHCMC) and a Community Affiliate (CA) from 2013 to 2015 were retrospectively reviewed. Patient demographics and preoperative comorbidities were compared. The variability of OR staff at each site was described. Four primary endpoints of the different OR phases were measured at the 2 locations and analyzed using standard statistical methods.
Results
The OR data of 74 cases of LRYGB at UHCMC and 106 cases at the CA were analyzed. Patient cohorts were comparable by age (45 ± 12 vs. 45 ± 10; p = 0.88), sex (82% vs. 79% female; p = 0.62), BMI (47.16 ± 7.33 vs. 45.91 ± 6.85; p = 0.25), and comorbidities. At CA, the teams who participated in LRYGB cases were fairly constant (8 circulating and scrub nurses, 4 anesthetists, 3 anesthesiologists), whereas at UHCMC there was great variability in the number of staff with 108 staff (39 circulating nurses, 57 scrub nurses/technicians, 59 anesthetists or anesthesia residents, 24 anesthesiologists) participated in LRYGB cases. There was no statistical difference between the total mean OR time and surgical time of the cases performed at the 2 sites (203 ± 59 min vs. 188 ± 39 min; p = 0.06; 152 ± 56 min; 145 ± 37 min; p = 0.36). However, the pre- and post-case times were longer at UHCMC compared to the CA (38 ± 9 min vs. 33 ± 6 min; p < 0.0001; 13 ± 6 min vs. 10 ± 3 min; p = 0.01).
Conclusion
The academic center has much greater variability in staff for these complex bariatric procedures. There was a trend toward longer OR times at the tertiary center as demonstrated by the difference in pre- and post-case times, but the consistent surgeon and assistant allowed for consistent surgical case time regardless of the setting. The implication of variability in OR staff can be overcome by the surgeon directing the procedure itself. The opportunity for improving the efficiency of bariatric surgery should focus on the perioperative care of the patient in OR that requires everyone to be familiar with the procedure.



Similar content being viewed by others
Change history
16 April 2020
This article was updated to correct Adel Alhaj Saleh���s name, incorrectly displayed as Adel A. Saleh. It is correct as displayed here: Adel (first name) Alhaj Saleh (last name).
References
Cheng H, Chen BP-H, Soleas IM, Ferko NC, Cameron CG, Hinoul P (2017) Prolonged operative duration increases risk of surgical site infections: a systematic review. Surg Infect 18(6):722–735. https://doi.org/10.1089/sur.2017.089
Campbell DA Jr, Henderson WG, Englesbe MJ, Hall BL, O'Reilly M, Bratzler D (2008) Surgical site infection prevention: the importance of operative duration and blood transfusion-results of the first American College of Surgeons-National Surgical Quality Improvement Program Best Practices Initiative. J Am Coll Surg 207(6):810–820. https://doi.org/10.1016/j.jamcollsurg.2008.08.018
Krell RW, Birkmeyer NJ, Reames BN, Carlin AM, Birkmeyer JD, Finks JF (2014) Effects of resident involvement on complication rates after laparoscopic gastric bypass. J Am Coll Surg 218(2):253–260. https://doi.org/10.1016/j.jamcollsurg.2013.10.014
Stepaniak PS, Vrijland WW, de Quelerij M, de Vries G, Heij C (2010) Working with a fixed operating room team on consecutive similar cases and the effect on case duration and turnover time. Arch Surg 145(12):1165–1170. https://doi.org/10.1001/archsurg.2010.255
Zheng B, Panton ONM, Al-Tayeb TA (2012) Operative length independently affected by surgical team size: data from 2 Canadian hospitals. Can J Surg 55(6):371–376. https://doi.org/10.1503/cjs.011311
He W, Ni S, Chen G, Jiang X, Zheng B (2014) The composition of surgical teams in the operating room and its impact on surgical team performance in China. Surg Endosc 28:1473. https://doi.org/10.1007/s00464-013-3318-4
Cassera MA, Zheng B, Martinec DV, Dunst CM, Swanstrom LL (2008) Surgical time independently affected by surgical team size. Am J Surg 198(2):216–222. https://doi.org/10.1016/j.amjsurg.2008.10.016
Doherty C, Nakoneshny SC, Harrop AR, Matthews T, Schrag C, McKenzie DC et al (2012) A standardized operative team for major head and neck cancer ablation and reconstruction. Plast Reconstr Surg 130(1):82–88. https://doi.org/10.1097/PRS.0b013e3182547e22
Morris LF, Romero Arenas MA, Cerny J, Berger JS, Borror CM, Ong M et al (2014) Streamlining variability in hospital charges for standard thyroidectomy: developing a strategy to decrease waste. Surgery 156(6):1441–1449. https://doi.org/10.1016/j.surg.2014.08.068. discussion 1449
Xu R, Carty MJ, Orgill DP, Lipsitz SR, Duclos A (2013) The teaming curve. Ann Surg 258(6):953–957. https://doi.org/10.1097/SLA.0b013e3182864ffe
Stepaniak PS, Christiaan H, Buise MP, Mannaerts GH, Smulders JF, Nienhuijs SW (2012) Bariatric surgery with operating room teams that stayed fixed during the day: a multicenter study analyzing the effects on patient outcomes, teamwork and safety climate, and procedure duration. Anesth Analg 115(6):1384–1392. https://doi.org/10.1213/ANE.0b013e31826c7fa6
Macario A (2010) What does one minute of operating room time cost? J Clin Anesth 22(4):233–236. https://doi.org/10.1016/j.jclinane.2010.02.003
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Wanda Lam, Dr. Gi Yoon Kim, Dr. Clayton Petro, Dr. Adel Alhaj Saleh and Dr. Leena Khaitan have no conflict of interest or financial ties relevant to this study to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article was updated to correct Adel Alhaj Saleh’s name, incorrectly displayed as Adel A. Saleh. It is correct as displayed here: Adel (first name) Alhaj Saleh (last name).
Rights and permissions
About this article
Cite this article
Lam, W., Kim, G.Y., Petro, C. et al. Bariatric efficiency at an academic tertiary care center. Surg Endosc 34, 2567–2571 (2020). https://doi.org/10.1007/s00464-020-07507-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07507-6