Abstract
Background
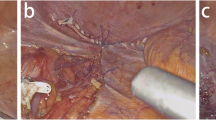
To investigate feasibility of laparoscopic abdominoperineal resection with pelvic peritoneum closure (LAPR-PPC) for lower rectal cancer.
Methods
LAPR-PPC has been used for lower rectal cancer in our institution since 2014. In this study, we retrospectively analyzed the data from 86 patients who underwent LAPR-PPC and compared with the data from 96 patients who underwent laparoscopic APR without PPC (LAPR) from January 2013 to December 2018.
Results
The rate of perineal surgical site infection (SSI) (18.75% (18/96) vs. 5.81% (5/86), p < 0.01), delayed (> 4 weeks) perineal healing (12.50% (12/96) vs. 3.49% (3/86), p = 0.027), ileus (7.29% (7/96) vs 1.16% (1/86), p = 0.044), and postoperative perineal hernia (PPH, 5.21% (5/96) vs. 0% (0/86), p = 0.032) were significantly lower in LAPR-PPC group than LAPR group. The patients in LAPR-PPC group had shorter hospitalization time (21.32 ± 11.95 days vs. 13.93 ± 11.51 days, p < 0.01).
Conclusions
PPC procedure enabled the reduction in perineal wound complications, ileus, PPH, and consequently shortened hospitalization time. LAPR-PPC is beneficial for the patients with lower rectal cancer.




Similar content being viewed by others
References
Fleshman J, Branda ME, Sargent DJ, Boller AM, George VV, Abbas MA, Peters WR Jr, Maun DC, Chang GJ, Herline A, Fichera A, Mutch MG, Wexner SD, Whiteford MH, Marks J, Birnbaum E, Margolin DA, Larson DW, Marcello PW, Posner MC, Read TE, Monson JRT, Wren SM, Pisters PWT, Nelson H (2019) Disease-free survival and local recurrence for laparoscopic resection compared with open resection of stage ii to iii rectal cancer: follow-up results of the ACOSOG Z6051 randomized controlled trial. Ann Surg 269:589–595
Stevenson ARL, Solomon MJ, Brown CSB, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Wilson K, Hague W, Simes J (2019) Disease-free survival and local recurrence after laparoscopic-assisted resection or open resection for rectal cancer: the Australasian laparoscopic cancer of the rectum randomized clinical trial. Ann Surg 269:596–602
Bertucci Zoccali M, Biondi A, Krane M, Kueberuwa E, Rizzo G, Persiani R, Coco C, Hurst RD, D'Ugo D, Fichera A (2015) Risk factors for wound complications in patients undergoing primary closure of the perineal defect after total proctectomy. Int J Colorectal Dis 30:87–95
Boelens PG, Heesakkers FF, Luyer MD, van Barneveld KW, de Hingh IH, Nieuwenhuijzen GA, Roos AN, Rutten HJ (2014) Reduction of postoperative ileus by early enteral nutrition in patients undergoing major rectal surgery: prospective, randomized, controlled trial. Ann Surg 259:649–655
Bertrand K, Lefevre JH, Creavin B, Luong M, Debove C, Voron T, Chafai N, Tiret E, Parc Y (2019) The management of perineal hernia following abdomino-perineal excision for cancer. Hernia. https://doi.org/10.1007/s10029-019-01927-7
Peirce C, Martin S (2016) Management of the perineal defect after abdominoperineal excision. Clin Colon Rectal Surg 29:160–167
de Campos FG, Habr-Gama A, Araujo SE, Sousa AH Jr, Nahas CR, Lupinacci RM, Nahas SC, Kiss DR, Gama-Rodrigues J (2005) Incidence and management of perineal hernia after laparoscopic proctectomy. Surg Laparosc Endosc Percutaneous Tech 15:366–370
Wang YW, Huang LY, Song CL, Zhuo CH, Shi DB, Cai GX, Xu Y, Cai SJ, Li XX (2015) Laparoscopic vs open abdominoperineal resection in the multimodality management of low rectal cancers. World J Gastroenterol 21:10174–10183
Foster JD, Tou S, Curtis NJ, Smart NJ, Acheson A, Maxwell-Armstrong C, Watts A, Singh B, Francis NK (2018) Closure of the perineal defect after abdominoperineal excision for rectal adenocarcinoma—ACPGBI position statement. Colorectal Dis 20(Suppl 5):5–23
Foster JD, Gash KJ, Carter FJ, West NP, Acheson AG, Horgan AF, Longman RJ, Coleman MG, Moran BJ, Francis NK (2014) Development and evaluation of a cadaveric training curriculum for low rectal cancer surgery in the English LOREC national development programme. Colorectal Dis 16:O308–319
Mathis KL, Larson DW, Dozois EJ, Cima RR, Huebner M, Haddock MG, Wolff BG, Nelson H, Pemberton JH (2012) Outcomes following surgery without radiotherapy for rectal cancer. Br J Surg 99:137–143
Blok RD, Musters GD, Borstlap WAA, Buskens CJ, Bemelman WA, Tanis PJ, Collaborative Dutch Snapshot Research Group (2018) Snapshot study on the value of omentoplasty in abdominoperineal resection with primary perineal closure for rectal cancer. Ann Surg Oncol 25:729–736
Tooley JE, Sceats LA, Bohl DD, Read B, Kin C (2018) Frequency and timing of short-term complications following abdominoperineal resection. J Surg Res 231:69–76
Woodfield J, Hulme-Moir M, Ly J (2017) A comparison of the cost of primary closure or rectus abdominis myocutaneous flap closure of the perineum after abdominoperineal excision. Colorectal Dis 19:934–941
Yasukawa D, Hori T, Kadokawa Y, Kato S, Aisu Y, Hasegawa S (2018) Trans-perineal minimally invasive surgery during laparoscopic abdominoperineal resection for low rectal cancer. Surg Endosc 32:437
Musters GD, Buskens CJ, Bemelman WA, Tanis PJ (2014) Perineal wound healing after abdominoperineal resection for rectal cancer: a systematic review and meta-analysis. Dis Colon Rectum 57:1129–1139
Melich G, Lim DR, Hur H, Min BS, Baik SH, Arena GO, Gordon PH, Kim NK (2016) Prevention of perineal hernia after laparoscopic and robotic abdominoperineal resection: review with illustrative case series of internal hernia through pelvic mesh. Can J Surg 59:54–58
Warembourg S, Labaki M, de Tayrac R, Costa P, Fatton B (2017) Reoperations for mesh-related complications after pelvic organ prolapse repair: 8-year experience at a tertiary referral center. Int Urogynecol J 28:1139–1151
Killeen S, Mannion M, Devaney A, Winter DC (2013) Omentoplasty to assist perineal defect closure following laparoscopic abdominoperineal resection. Colorectal Dis 15:e623–626
Killeen S, Devaney A, Mannion M, Martin ST, Winter DC (2013) Omental pedicle flaps following proctectomy: a systematic review. Colorectal Dis 15:e634–645
Feng B, Lu J, Zhang S, Yan X, Li J, Xue P, Wang M, Lu A, Ma J, Zang L, Dong F, He Z, Yue F, Sun J, Hong X, Zheng M (2017) Laparoscopic abdominoperineal excision with trans-abdominal individualized levator transection: interim analysis of a randomized controlled trial. Colorectal Dis 19:O246–O252
Foster JD, Pathak S, Smart NJ, Branagan G, Longman RJ, Thomas MG, Francis N (2012) Reconstruction of the perineum following extralevator abdominoperineal excision for carcinoma of the lower rectum: a systematic review. Colorectal Dis 14:1052–1059
Martijnse IS, Holman F, Nieuwenhuijzen GA, Rutten HJ, Nienhuijs SW (2012) Perineal hernia repair after abdominoperineal rectal excision. Dis Colon Rectum 55:90–95
Balla A, Batista Rodriguez G, Buonomo N, Martinez C, Hernandez P, Bollo J, Targarona EM (2017) Perineal hernia repair after abdominoperineal excision or extralevator abdominoperineal excision: a systematic review of the literature. Tech Coloproctol 21:329–336
Teramura K, Watanabe Y, Takeuchi S, Nakamura F, Hirano S (2018) Laparoscopic repair with cone-shaped mesh implantation for perineal hernia occurred after laparoscopic abdominoperineal resection. Int J Surg Case Rep 49:115–117
Mjoli M, Sloothaak DA, Buskens CJ, Bemelman WA, Tanis PJ (2012) Perineal hernia repair after abdominoperineal resection: a pooled analysis. Colorectal Dis 14:e400–406
Sayers AE, Patel RK, Hunter IA (2015) Perineal hernia formation following extralevator abdominoperineal excision. Colorectal Dis 17:351–355
Yang T, Wei M, Deng X, Meng W, Wang Z (2019) A Novel laparoscopic technique with a bladder peritoneum flap closure for pelvic cavity for patients with rigid pelvic peritoneum after neoadjuvant radiotherapy in laparoscopic extralevator abdominoperineal excision. Dis Colon Rectum 62:5
Funding
This work was supported by Shanghai Municipal Commission of Health and Family Planning Program (201640030), Shanghai translational medicine collaborative innovation center program (TM201701), Shanghai Shen-kang Hospital Development Centre (16CR1011A).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Diclosures
Xialin Yan, Hao Su, Sen Zhang, Leqi Zhou, Jiaoyang Lu, Xiao Yang, Jianwen Li, Pei Xue, Zirui He, Mingliang Wang, Aiguo Lu, Junjun Ma, Lu Zang, Cai Zhenghao, Jing Sun, Hiju Hong, Minhua Zheng, and Bo Feng have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yan, X., Su, H., Zhang, S. et al. Pelvic peritoneum closure reduces postoperative complications of laparoscopic abdominoperineal resection: 6-year experience in single center. Surg Endosc 35, 406–414 (2021). https://doi.org/10.1007/s00464-020-07414-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07414-w