Abstract
Background
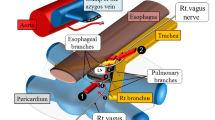
Although thoracoscopic esophagectomy in the prone position (TEPP) has become a standard procedure for esophageal cancer surgery, upper mediastinal lymph node dissection (UMLND) on the left side remains an issue. We have recently developed a new standardized approach to left UMLND in TEPP based on the microanatomy of the membranes and layers with the aim of achieving quick and safe surgery. The purpose of this study was to establish and evaluate our new standardized procedure in left UMLND.
Patients and methods
Patients were divided into 2 groups: a pre-standardization group (n = 100) and a post-standardization group (n = 100). Eventually, 83 paired cases were matched using propensity score matching. In our new standardized procedure, left UMLND was performed while focusing on the visceral sheath, vascular sheath, and the fusion layer between them using a magnified view.
Results
The thoracoscopic operative time was significantly shorter (P < 0.001) in the post-standardization group [n = 83; 209.0 (176.0–235.0) min] than in the pre-standardization group [n = 83; 235.5 (202.8–264.5) min]. No significant differences were found in the number of mediastinal lymph nodes dissected or intraoperative blood loss between the two groups. There was a tendency for the total postoperative morbidity to decrease in the post-standardization group. Furthermore, the left recurrent laryngeal nerve palsy rate was significantly lower in the post-standardization group (18.1% to 8.7%, P = 0.015).
Conclusion
Microanatomy-based standardization contributes to safe and efficient left UMLND.






Similar content being viewed by others
References
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Akiyama H, Tsurumaru MA, Kawamura T, Ono Y (1981) Principles of Surgical Treatment for Carcinoma of the Esophagus AnalysisofLymph Node Involvement. Ann Surg 194:438–445
Akiyama H, Tsurumaru M, Udagawa H, Kajiyama Y (1994) Radical Lymph Node Dissection for CanceroftheThoracicEsophagus. Ann Surg 220:364–373
Fujita H, Sueyoshi S, Tanaka T, Fujii T, Toh U, Mine T, Sasahara H, Sudo T, Matono S, Yamana H, Shirouzu K (2003) Optimal lymphadenectomy for squamous cell carcinoma in the thoracic esophagus: comparing the short- and long-term outcome among the four types of lymphadenectomy. World J Surg 27:571–579
Igaki H, Tachimori Y, Kato H (2004) Improved survival for patients with upper and/or middle mediastinal lymph node metastasis of squamous cell carcinoma of the lower thoracic esophagus treated with 3-field dissection. Ann Surg 239:483–490
Watson A (1994) Operable esophageal cancer: current results from the West. World J Surg 18:361–366
Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA (2003) Complications and costs after high-risk surgery: where should we focus quality improvement initiatives? J Am Coll Surg 196:671–678
Atkins BZ, Shah AS, Hutcheson KA, Mangum JH, Pappas TN, Harpole DH, Amico TA (2004) Reducing hospital morbidity and mortality following esophagectomy. Ann Thorac Surg 78:1170–1176; discussion 1170–1176
Cuschieri A, Shimi S, Banting S (1992) Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 37:7–11
Cuschieri A (1993) Endoscopic subtotal oesophagectomy for cancer using the right thoracoscopic approach. Surg Oncol 2(Suppl 1):3–11
Cuschieri A (1994) Thoracoscopic subtotal oesophagectomy. Endosc Surg Allied Technol 2:21–25
Akaishi T, Kaneda I, Higuchi N, Kuriya Y, Kuramoto J, Toyoda T, Wakabayashi A (1996) Thoracoscopic en bloc total esophagectomy with radical mediastinal lymphadenectomy. J Thorac Cardiovasc Surg 112:1533–1540
Osugi H, Takemura M, Higashino M, Takada N, Lee S, Kinoshita H (2003) A comparison of video-assisted thoracoscopic oesophagectomy and radical lymph node dissection for squamous cell cancer of the oesophagus with open operation. Br J Surg 90:108–113
Palanivelu C, Prakash A, Senthilkumar R, Senthilnathan P, Parthasarathi R, Rajan PS, Venkatachlam S (2006) Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position–experience of 130 patients. J Am Coll Surg 203:7–16
Noshiro H, Iwasaki H, Kobayashi K, Uchiyama A, Miyasaka Y, Masatsugu T, Koike K, Miyazaki K (2010) Lymphadenectomy along the left recurrent laryngeal nerve by a minimally invasive esophagectomy in the prone position for thoracic esophageal cancer. Surg Endosc 24:2965–2973
Tsujimoto H, Takahata R, Nomura S, Yaguchi Y, Kumano I, Matsumoto Y, Yoshida K, Horiguchi H, Hiraki S, Ono S, Yamamoto J, Hase K (2012) Video-assisted thoracoscopic surgery for esophageal cancer attenuates postoperative systemic responses and pulmonary complications. Surgery 151:667–673
Ozawa S, Ito E, Kazuno A, Chino O, Nakui M, Yamamoto S, Shimada H, Makuuchi H (2013) Thoracoscopic esophagectomy while in a prone position for esophageal cancer: a preceding anterior approach method. Surg Endosc 27:40–47
Yatabe T, Kitagawa H, Yamashita K, Hanazaki K, Yokoyama M (2013) Comparison of the perioperative outcome of esophagectomy by thoracoscopy in the prone position with that of thoracotomy in the lateral decubitus position. Surg Today 43:386–391
Shirakawa Y, Noma K, Maeda N, Katsube R, Tanabe S, Ohara T, Sakurama K, Fujiwara T (2014) Assistant-based standardization of prone position thoracoscopic esophagectomy. Acta Med Okayama 68:111–117
Oshikiri T, Yasuda T, Harada H, Goto H, Oyama M, Hasegawa H, Ohara T, Sendo H, Nakamura T, Fujino Y, Tominaga M, Kakeji Y (2015) A new method (the "Bascule method") for lymphadenectomy along the left recurrent laryngeal nerve during prone esophagectomy for esophageal cancer. Surg Endosc 29:2442–2450
Akagawa S, Hosogi H, Yoshimura F, Kawada H, Kanaya S (2018) Mesenteric excision for esophageal cancer surgery: based on the concept of mesotracheoesophagus. Int Cancer Conf J 7:117–120
Parsons FG (1910) On the carotid sheath and other fascial planes. J Anat Physiol 44:153–155
Grodinsky M, Holyoke EA (1938) The fasciae and fascial spaces of the head, neck and adjacent regeions. Am J Anat 63:367–408
Range RL, Woodburne RT (1964) The gross and microscopic anatomy of the transverse cervical ligament. Am J Obstet Gynecol 90:460–467
Salassa JR, Pearson BW, Payne WS (1977) Gross and microscopical blood supply of the trachea. Ann Thorac Surg 24:100–107
Japanese Classification of Esophageal Cancer (2017) 11th Edition: part I. Esophagus 14:1–36
Japanese Classification of Esophageal Cancer (2017) 11th Edition: part II and III. Esophagus 14:37–65
Brierley JD, Gospodarowicz MK, Wittekind C (2017) TNM classification of malignant tumors (UICC international union against cancer), 8th edn. Wiley-Blackwell, Oxford
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal Dis 11:354–364
Heald RJ (1988) The 'Holy Plane' of rectal surgery. J R Soc Med 81:503–508
Havenga K, Grossmann I, DeRuiter M, Wiggers T (2007) Definition of total mesorectal excision, including the perineal phase: technical considerations. Dig Dis 25:44–50
Cuesta MA, Weijs TJ, Bleys RL, van Hillegersberg R, van Berge Henegouwen MI, Gisbertz SS, Ruurda JP, Straatman J, Osugi H, van der Peet DL (2015) A new concept of the anatomy of the thoracic oesophagus: the meso-oesophagus. Observational study during thoracoscopic esophagectomy. Surg Endosc 29:2576–2582
Tokairin Y, Nakajima Y, Kawada K, Hoshino A, Okada T, Ryotokuji T, Okuda M, Kume Y, Kawamura Y, Yamaguchi K, Nagai K, Akita K, Kinugasa Y (2018) Histological study of the thin membranous structure made of dense connective tissue around the esophagus in the upper mediastinum. Esophagus 15:272–280
Hayashi S (2007) Histology of the human carotid sheath revisited. Okajimas Folia Anat Jpn 84:49–60
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Yasuhiro Shirakawa, Kazuhiro Noma, Naoaki Maeda, Shunsuke Tanabe, Kazufumi Sakurama, and Toshiyoshi Fujiwara have no conflicts of interest or financial ties to disclose.
Ethical approval
All procedures followed were in accordance with the Helsinki Declaration of 1964 and its later versions. This study was approved by the Ethics Committee of Okayama University Hospital (1811–009).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shirakawa, Y., Noma, K., Maeda, N. et al. Microanatomy-based standardization of left upper mediastinal lymph node dissection in thoracoscopic esophagectomy in the prone position. Surg Endosc 35, 349–357 (2021). https://doi.org/10.1007/s00464-020-07407-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07407-9