Abstract
Background
Pancreatic neuroendocrine neoplasms (PanNEN) are ideal entities for minimally invasive surgery. The advantage of the laparoscopic approach in terms of complications, length of stay (LOS) and cosmetic results has been previously demonstrated. However, scarce data are available on long-term oncological outcomes. Aim of this study was to compare short-term postoperative outcomes, pathological findings and long-term oncological results of minimally invasive distal pancreatectomy (MIDP) and open distal pancreatectomy (ODP) for PanNEN.
Methods
Patients who underwent ODP or MIDP for nonfunctioning PanNEN (NF-PanNEN) were retrospectively analyzed. Inverse probability of treatment weighting using propensity score was performed to compare the outcomes of MIDP and ODP.
Results
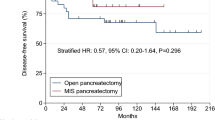
Overall, 124 patients were included in the study: 84 underwent OPD, whereas 40 were submitted to MIDP. The rate of high-grade postoperative complications was significantly lower in the MIDP group (p = 0.005, grade of complication with highest estimated probability 0 vs 2) and the postoperative LOS was significantly shorter after MIDP (p < 0.001, estimated days 8 versus 10). The number of examined lymph nodes (ELN) in the ODP group was significantly higher (p = 0.0036, estimated number of ELN 13 vs 10). Similar disease-free survival and overall survival were reported for the two groups (p = 0.234 and p = 0.666, respectively).
Conclusions
Although MIDP for PanNEN seems to be associated with a lower number of ELN, long-term survival is not influenced by the type of surgical approach. MIDP is advantageous in terms of postoperative complications and LOS, but prospective studies are needed to confirm the overall oncological quality of resection in this group of neoplasms.


Similar content being viewed by others
References
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, Shih T, Yao JC (2017) Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol 3(10):1335–1342
Haugvik SP, Marangos IP, Rosok BI, Pomianowska E, Gladhaug IP, Mathisen O, Edwin B (2013) Long-term outcome of laparoscopic surgery for pancreatic neuroendocrine tumors. World J Surg 37(3):582–590
Fernandez-Cruz L, Blanco L, Cosa R, Rendon H (2008) Is laparoscopic resection adequate in patients with neuroendocrine pancreatic tumors? World J Surg 32(5):904–917
Drymousis P, Raptis DA, Spalding D, Fernandez-Cruz L, Menon D, Breitenstein S, Davidson B, Frilling A (2014) Laparoscopic versus open pancreas resection for pancreatic neuroendocrine tumours: a systematic review and meta-analysis. HPB (Oxford) 16(5):397–406
Han SH, Han IW, Heo JS, Choi SH, Choi DW, Han S, You YH (2018) Laparoscopic versus open distal pancreatectomy for nonfunctioning pancreatic neuroendocrine tumors: a large single-center study. Surg Endosc 32(1):443–449
Xourafas D, Tavakkoli A, Clancy TE, Ashley SW (2015) Distal pancreatic resection for neuroendocrine tumors: is laparoscopic really better than open? J Gastrointest Surg 19(5):831–840
Soper NJ, Brunt LM, Dunnegan DL, Meininger TA (1994) Laparoscopic distal pancreatectomy in the porcine model. Surg Endosc 8(1):57–60 (discussion 60–51)
Edwin B, Sahakyan MA, Abu Hilal M, Besselink MG, Braga M, Fabre JM, Fernandez-Cruz L, Gayet B, Kim SC, Khatkov IE (2017) Laparoscopic surgery for pancreatic neoplasms: the European association for endoscopic surgery clinical consensus conference. Surg Endosc 31(5):2023–2041
Casadei R, Ricci C, Pacilio CA, Ingaldi C, Taffurelli G, Minni F (2018) Laparoscopic distal pancreatectomy: which factors are related to open conversion? Lessons learned from 68 consecutive procedures in a high-volume pancreatic center. Surg Endosc 32(9):3839–3845
Braga M, Pecorelli N, Ferrari D, Balzano G, Zuliani W, Castoldi R (2015) Results of 100 consecutive laparoscopic distal pancreatectomies: postoperative outcome, cost-benefit analysis, and quality of life assessment. Surg Endosc 29(7):1871–1878
van Hilst J, Korrel M, de Rooij T, Lof S, Busch OR, Groot Koerkamp B, Kooby DA, van Dieren S, Abu Hilal M, Besselink MG (2019) Oncologic outcomes of minimally invasive versus open distal pancreatectomy for pancreatic ductal adenocarcinoma: a systematic review and meta-analysis. Eur J Surg Oncol 45(5):719–727
de Rooij T, Klompmaker S, Abu Hilal M, Kendrick ML, Busch OR, Besselink MG (2016) Laparoscopic pancreatic surgery for benign and malignant disease. Nat Rev Gastroenterol Hepatol 13(4):227–238
de Rooij T, van Hilst J, van Santvoort H, Boerma D, van den Boezem P, Daams F, van Dam R, Dejong C, van Duyn E, Dijkgraaf M et al (2019) Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg 269(1):2–9
van Hilst J, de Rooij T, Abu Hilal M, Asbun HJ, Barkun J, Boggi U, Busch OR, Conlon KC, Dijkgraaf MG, Han HS et al (2017) Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB (Oxford) 19(3):190–204
de Rooij T, Besselink MG, Shamali A, Butturini G, Busch OR, Edwin B, Troisi R, Fernandez-Cruz L, Dagher I, Bassi C et al (2016) Pan-European survey on the implementation of minimally invasive pancreatic surgery with emphasis on cancer. HPB (Oxford) 18(2):170–176
Abu Hilal M, Richardson JR, de Rooij T, Dimovska E, Al-Saati H, Besselink MG (2016) Laparoscopic radical 'no-touch' left pancreatosplenectomy for pancreatic ductal adenocarcinoma: technique and results. Surg Endosc 30(9):3830–3838
Sahakyan MA, Kazaryan AM, Rawashdeh M, Fuks D, Shmavonyan M, Haugvik SP, Labori KJ, Buanes T, Rosok BI, Ignjatovic D et al (2016) Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: results of a multicenter cohort study on 196 patients. Surg Endosc 30(8):3409–3418
van Hilst J, de Rooij T, Klompmaker S, Rawashdeh M, Aleotti F, Al-Sarireh B, Alseidi A, Ateeb Z, Balzano G, Berrevoet F et al (2019) Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a pan-european propensity score matched study. Ann Surg 269(1):10–17
Stauffer JA, Coppola A, Mody K, Asbun HJ (2016) Laparoscopic Versus open distal pancreatectomy for pancreatic adenocarcinoma. World J Surg 40(6):1477–1484
Tamburrino D, Partelli S, Renzi C, Crippa S, Muffatti F, Perali C, Parisi A, Randolph J, Fusai GK, Cirocchi R et al (2017) Systematic review and meta-analysis on laparoscopic pancreatic resections for neuroendocrine neoplasms (PNENs). Expert Rev Gastroenterol Hepatol 11(1):65–73
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161(3):584–591
Rindi G, Kloppel G, Alhman H, Caplin M, Couvelard A, de Herder WW, Erikssson B, Falchetti A, Falconi M, Komminoth P et al (2006) TNM staging of foregut (neuro)endocrine tumors: a consensus proposal including a grading system. Virchows Arch 449(4):395–401
Lloyd RV, Osamura RY, Kloppel GRJ (2017) WHO classification of tumours of endocrine organs, 4th edn. IARC Press, Lyon, France, p 10
Schemper M, Smith TL (1996) A note on quantifying follow-up in studies of failure time. Control Clin Trials 17(4):343–346
Austin PC, Stuart EA (2015) Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 34(28):3661–3679
Normand ST, Landrum MB, Guadagnoli E, Ayanian JZ, Ryan TJ, Cleary PD, McNeil BJ (2001) Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol 54(4):387–398
Lopez CL, Albers MB, Bollmann C, Manoharan J, Waldmann J, Fendrich V, Bartsch DK (2016) Minimally invasive versus open pancreatic surgery in patients with multiple endocrine neoplasia type 1. World J Surg 40(7):1729–1736
Mintziras I, Keck T, Werner J, Fichtner-Feigl S, Wittel U, Senninger N, Vowinkel T, Koninger J, Anthuber M, Geissler B et al (2019) Implementation of current ENETS guidelines for surgery of small (%3c/=2 cm) pancreatic neuroendocrine neoplasms in the german surgical community: an analysis of the prospective DGAV StuDoQ|Pancreas Registry. World J Surg 43(1):175–182
Falconi M, Eriksson B, Kaltsas G, Bartsch DK, Capdevila J, Caplin M, Kos-Kudla B, Kwekkeboom D, Rindi G, Kloppel G et al (2016) ENETS Consensus guidelines update for the management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology 103(2):153–171
Partelli S, Bartsch DK, Capdevila J, Chen J, Knigge U, Niederle B, Nieveen van Dijkum EJM, Pape UF, Pascher A, Ramage J et al (2017) ENETS Consensus guidelines for standard of care in neuroendocrine tumours: surgery for small intestinal and pancreatic neuroendocrine tumours. Neuroendocrinology 105(3):255–265
Acknowledgements
Dr Valentina Andreasi PhD studentship and Dr Francesca Muffatti research fellowship were supported by Ms Gioja Bianca Costanza legacy donation. Authors thank the ERN EURACAN initiative.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Stefano Partelli, Valentina Andreasi, Paola Maria Vittoria Rancoita, Eduardo Perez-Sanchez, Francesca Muffatti, Gianpaolo Balzano, Stefano Crippa, Clelia Di Serio, and Massimo Falconi have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Partelli, S., Andreasi, V., Rancoita, P.M.V. et al. Outcomes after distal pancreatectomy for neuroendocrine neoplasms: a retrospective comparison between minimally invasive and open approach using propensity score weighting. Surg Endosc 35, 165–173 (2021). https://doi.org/10.1007/s00464-020-07375-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07375-0