Abstract
Background and aims
Currently available endoscopic or minimally invasive antireflux modalities are not widely accepted due to high procedure cost or inconsistent results. Therefore, a simpler and less technically demanding method is required. We evaluated the feasibility and efficacy of new endoscopic antireflux method (the Ripple Procedure) using functional lumen imaging probe (FLIP).
Methods
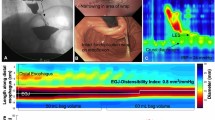
This 5-week survival study included 10 domestic pigs (control, n = 4; experimental [Ripple], n = 6). The procedure includes the following steps: (i) semicircular marking along the lesser curvature of the cardia; (ii) submucosal injection; and (iii) semicircular mucosal incision along the marking. Endoscopic and FLIP evaluations were performed preoperatively and on postoperative days (PODs) 14 and 35. Technical feasibility was evaluated, and FLIP parameters, including the distensibility index (DI) at the esophagogastric junction (EGJ) and histopathological findings, were compared between groups.
Results
The median procedure time was 28 (23.5–33.8) min. There was no significant difference in dysphagia score and body weight between groups. On POD 35, the Ripple group showed significantly lower EGJ DI at 30 mL [2.0 (1.3–2.5) vs 4.9 (2.7–5.0), P = 0.037]. The EGJ DI was significantly reduced at 30 mL, compared with that at the baseline level [− 59.0% (− 68.8% to − 32.1%) vs 27.8% (− 26.3% to 83.1%), P = 0.033]. Histologic evaluation revealed submucosal granulation tissues near the mucosal incision site, with increased intervening fibrosis between lower esophageal sphincter fibers in the Ripple group.
Conclusion
The EGJ DI significantly decreased after the Ripple Procedure; hence, the procedure appears to be feasible and effective in this porcine model.




Similar content being viewed by others
References
Pandolfino JE, Krishnan K (2014) Do endoscopic antireflux procedures fit in the current treatment paradigm of gastroesophageal reflux disease? Clin Gastroenterol Hepatol 12:544–554
Nabi Z, Reddy DN (2016) Endoscopic management of gastroesophageal reflux disease: revisited. Clin Endosc 49:408–416
Arts J, Tack J, Galmiche JP (2004) Endoscopic antireflux procedures. Gut 53:1207–1214
Iizuka H, Kakizaki S, Sohara N et al (2010) Stricture after endoscopic submucosal dissection for early gastric cancers and adenomas. Dig Endosc 22:282–288
Inoue H, Ito H, Ikeda H et al (2014) Anti-reflux mucosectomy for gastroesophageal reflux disease in the absence of hiatus hernia: a pilot study. Ann Gastroenterol 27:346–351
Perretta S, Dallemagne B, McMahon B, D’Agostino J, Marescaux J (2011) Video. Improving functional esophageal surgery with a “smart” bougie: endoflip. Surg Endosc 25:3109
Ilczyszyn A, Botha AJ (2014) Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus 27:637–644
Hoppo T, McMahon BP, Witteman BP et al (2011) Functional lumen imaging probe to assess geometric changes in the esophagogastric junction following endolumenal fundoplication. J Gastrointest Surg 15:1112–1120
McMahon BP, Frokjaer JB, Drewes AM, Gregersen H (2004) A new measurement of oesophago-gastric junction competence. Neurogastroenterol Motil 16:543–546
DeHaan RK, Davila D, Frelich MJ, Gould JC (2017) Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc 31:193–198
Hirano I, Pandolfino JE, Boeckxstaens GE (2017) Functional lumen imaging probe for the management of esophageal disorders: expert review from the clinical practice updates Committee of the AGA Institute. Clin Gastroenterol Hepatol 15:325–334
Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ (2010) Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc 72:272–278
Sharma P, Kozarek R (2010) Practice parameters committee of american college of gastroenterology. Role of esophageal stents in benign and malignant diseases. Am J Gastroenterol 105:258–273
Hedberg HM, Kuchta K, Ujiki MB (2019) First experience with banded anti-reflux mucosectomy (ARMS) for GERD: feasibility, safety, and technique (with Video). J Gastrointest Surg 23:1274–1278
Vegesna AK, Braverman AS, Miller LS et al (2010) Comparison of human and porcine gastric clasp and sling fiber contraction by M2 and M3 muscarinic receptors. Am J Physiol Gastrointest Liver Physiol 298:G530–534
Vicente Y, Da Rocha C, Yu J et al (2001) Architecture and function of the gastroesophageal barrier in the piglet. Dig Dis Sci 46:1899–1908
Chen JW, Rubenstein JH (2017) Esophagogastric junction distensibility assessed using the functional lumen imaging probe. World J Gastroenterol 23:1289–1297
Rinsma NF, Smeets FG, Bruls DW et al (2014) Effect of transoral incisionless fundoplication on reflux mechanisms. Surg Endosc 28:941–949
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Hyunsoo Chung, Se Hoon Kim, and Sung Kwan Shin have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chung, H., Kim, S.H. & Shin, S.K. A potential simple endoscopic antireflux method, “the Ripple Procedure” to reduce distensibility at the esophagogastric junction in a porcine model. Surg Endosc 34, 5017–5022 (2020). https://doi.org/10.1007/s00464-019-07296-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07296-7