Abstract
Introduction
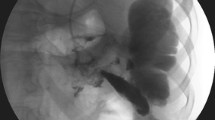
Internal drainage of walled of necrosis of pancreas has been considered as the standard of care. For symptomatic walled off necrosis (WON) of pancreas with the advent of laparoscopy and refinement of techniques and instrumentation, laparoscopic internal drainage is becoming the standard surgical drainage procedure for these patients. However, there is a dearth of literature regarding outcomes following laparoscopic drainage. Most of the studies have small number of patients with limited follow-up. We in this study describe our experience of laparoscopic internal drainage of walled off necrosis over the last 13 years.
Materials and methods
This is a retrospective analysis of a prospectively maintained database. All patients with WON undergoing laparoscopic internal drainage between January 2005 and December 2018 were included. Primary outcome measure was successful drainage. Secondary outcome measures included morbidity, hospital stay, re-intervention rate and mortality. Patients were followed up post-operatively at 1 week, 4 weeks, 3 months and then annually thereafter. Ultrasonography was done periodically for the assessment of cyst resolution.
Results
Between 2005 and 2018, 154 surgical drainage procedures were performed for symptomatic pseudocyst/walled off necrosis. Out of these, 134 underwent laparoscopic drainage; 129 patients (96.3%) underwent laparoscopic cystogastrostomy and 5 (3.7%) underwent laparoscopic cystojejunostomy. Majority of the patients were male (male:female = 6:1) with a mean age of 36 ± 12.9 years (range 15–58 years). The mean operative time was 94 min (range 64–144 min). There were three conversions because of intra-operative bleeding. The overall post-operative morbidity was 8.9%. The average hospital stay was 4.4 days (2–19 days). The mean duration of follow-up was 5.5 years (range 6 months–13 years). Complete cyst resolution was achieved in 95.5% (n = 128) patients. There has been no mortality till date.
Conclusion
In conclusion, laparoscopic internal drainage is a very effective technique for drainage of WON with an excellent success rate.
Similar content being viewed by others
References
Isayama H, Nakai Y, Rerknimitr R, Khor C, Lau J, Wang H-P et al (2016) Asian consensus statements on endoscopic management of walled-off necrosis. Part 1: epidemiology, diagnosis, and treatment. J Gastroenterol Hepatol 31(9):1546–1554
Lerch MM, Stier A, Wahnschaffe U, Mayerle J (2009) Pancreatic pseudocysts: observation, endoscopic drainage, or resection? Dtsch Arzteblatt Int 106(38):614–621
Aljarabah M, Ammori BJ (2007) Laparoscopic and endoscopic approaches for drainage of pancreatic pseudocysts: a systematic review of published series. Surg Endosc 21(11):1936–1944
Wu T-M, Jin Z-K, He Q, Zhao X, Kou J-T, Fan H (2017) Treatment of retrogastric pancreatic pseudocysts by laparoscopic transgastric cystogastrostomy. J Huazhong Univ Sci Technol Med Sci Hua Zhong Ke Ji Xue Xue Bao Yi Xue Ying Wen Ban Huazhong Keji Daxue Xuebao Yixue Yingdewen Ban 37(5):726–731
Yu Z, Wu Z, Han J, Zhou H, Jiao Z (2014) Laparoscopic cystogastrostomy with posterior approach for pancreatic pseudocyst drainage. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 39(10):1035–1038
Malik AA, Isnain HG, Khan A, Toor AA, Nawaz A, Mansoor R et al (2015) Laparoscopic cystgastrostomy: a Pakistani perspective. JPMA J Pak Med Assoc 65(5):565–568
Garg PK, Meena D, Babu D, Padhan RK, Dhingra R, Krishna A, Kumar S, Misra MC, Bansal VK (2019) Endoscopic versus laparoscopic drainage of pseudocyst and walled-off necrosis following acute pancreatitis: a randomized trial. Surg Endosc. https://doi.org/10.1007/s00464-019-06866-z
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG et al (2013) Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut 62(1):102–111
Mehta R, Suvarna D, Sadasivan S, John A, Raj V, Nair P et al (2004) Natural course of asymptomatic pancreatic pseudocyst: a prospective study. Indian J Gastroenterol 23(4):140–142
Mori T, Abe N, Sugiyama M, Atomi Y (2002) Laparoscopic pancreatic cystgastrostomy. J Hepatobiliary Pancreat Surg 9(5):548–554
Rosso E, Alexakis N, Ghaneh P, Lombard M, Smart HL, Evans J et al (2003) Pancreatic pseudocyst in chronic pancreatitis: endoscopic and surgical treatment. Dig Surg 20(5):397–406
Varadarajulu S, Bang JY, Sutton BS, Trevino JM, Christein JD, Wilcox CM (2013) Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology 145(3):583–590.e1
Bhattacharya D, Ammori BJ (2003) Minimally invasive approaches to the management of pancreatic pseudocysts: review of the literature. Surg Laparosc Endosc Percutan Tech 13(3):141–148
Melman L, Azar R, Beddow K, Brunt LM, Halpin VJ, Eagon JC et al (2009) Primary and overall success rates for clinical outcomes after laparoscopic, endoscopic, and open pancreatic cystgastrostomy for pancreatic pseudocysts. Surg Endosc 23(2):267–271
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Virinder Kumar Bansal, Asuri Krishna, Om Prakash Prajapati, Aditya Baksi, Subodh Kumar, Pramod Garg and Mahesh Chandra Misra have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bansal, V.K., Krishna, A., Prajapati, O.P. et al. Outcomes following laparoscopic internal drainage of walled off necrosis of pancreas: experience of 134 cases from a tertiary care centre. Surg Endosc 34, 5117–5121 (2020). https://doi.org/10.1007/s00464-019-07282-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07282-z