Abstract
Background
The feasibility of endoscopic dissection for gastric gastrointestinal stromal tumor (gGIST) between 2 and 5 cm in size has been demonstrated. However, its impact on short-term and long-term outcomes, compared with laparoscopic resection, is unknown. The purpose of this study was to compare short-term and long-term outcomes between laparoscopic resection and endoscopic dissection for 2–5-cm gGIST.
Methods
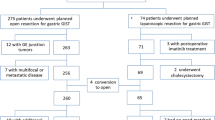
A case-matched study was performed using the propensity score. To overcome selection bias, we performed a 1:1 match using six covariates, including age, sex, BMI, ASA score, tumor size, and tumor location. Short-term and long-term outcomes between laparoscopic resection and endoscopic dissection were compared.
Results
A total of 210 patients with 2–5-cm gGIST were enrolled between 2006 and 2017 in our gastrointestinal center. According to the intention-to-treat approach, 165 patients underwent laparoscopic resection, and 45 patients underwent endoscopic dissection. After the propensity score, 45 pairs were balanced and analyzed. There was no significant difference in the baseline characteristics between the laparoscopic and endoscopic groups after matching. The rate of complications was significantly higher in the endoscopic group compared with the laparoscopic group (P < 0.001). Perforations occurred in 16 patients in the endoscopic group (16/45, 35.6%). The postoperative hospital stay was significantly longer in the endoscopic group compared with the laparoscopic group (P < 0.001). There was no significant difference between the two groups in disease-free survival or overall survival.
Conclusion
Laparoscopic resection is better than endoscopic dissection for 2–5-cm gGIST because of the lower complication rate and shorter hospital stay.
Visual abstract




Similar content being viewed by others
References
Joensuu H, Hohenberger P, Corless CL (2013) Gastrointestinal stromal tumour. Lancet 382:973–983
ESMO Guidelines Committee and EURACAN (2018) Gastrointestinal stromal tumour: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 29(Supplement 4):iv267
Nishida T, Blay JY, Hirota S, Kitagawa Y, Kang YK (2016) The standard diagnosis, treatment, and follow-up of gastrointestinal stromal tumors based on guidelines. Gastric Cancer 19:3–14
Chinese Society of Clinical Oncology (2017) Chinese consensus guidelines for diagnosis and management of gastrointestinal stromal tumor. Chin J Cancer Res 29:281–293
Nishimura J, Nakajima K, Omori T, Takahashi T, Nishitani A, Ito T, Nishida T (2007) Surgical strategy for gastric gastrointestinal stromal tumors: laparoscopic vs. open resection. Surg Endosc 21:875–878
Zheng L, Ding W, Zhou D, Lu L, Yao L (2014) Laparoscopic versus open resection for gastric gastrointestinal stromal tumors: a meta-analysis. Am Surg 80:48–56
Chen K, Zhou YC, Mou YP, Xu XW, Jin WW, Ajoodhea H (2015) Systematic review and meta-analysis of safety and efficacy of laparoscopic resetion for gastrointestinal stromal tumors of the stomach. Surg Endosc 29:355–367
Chen QL, Pan Y, Cai JQ, Wu D, Chen K, Mou YP (2014) Laparoscopic versus open resection for gastric gastrointestinal stromal tumors: an updated systematic review and meta-analysis. World J Surg Oncol 12:206–219
Ohtani H, Maeda K, Noda E, Nagahara H, Shibutani M, Ohira M, Muguruma K, Tanaka H, Kubo N, Toyokawa T, Sakurai K, Yamashita Y, Yamamoto A, Hirakawa K (2013) Meta-analysis of laparoscopic and open surgery for gastric gastrointestinal stromal tumor. Anticancer Res 33:5031–5041
Liang JW, Zheng ZC, Zhang JJ, Zhang T, Zhao Y, Yang W, Liu YQ (2013) Laparoscopic versus open gastric resections for gastric gastrointestinal stromal tumors: a meta-analysis. Surg Laparosc Endosc Percutan Tech 23:378–387
Koh YX, Chok AY, Zheng HL, Tan CS, Chow PK, Wong WK, Goh BK (2013) A systematic review and meta-analysis comparing laparoscopic versus open gastric resections for gastrointestinal stromal tumors of the stomach. Ann Aurg Oncol 20:3549–3560
The National Comprehensive Cancer Network (2018) Soft tissue sarcoma, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 16:536–563
Otani Y, Furukawa T, Yoshida M, Saikawa Y, Wada N, Ueda M, Kubota T, Mukai M, Kameyama K, Sugino Y, Kumai K, Kitajima M (2006) Operative indications for relatively small (2–5 cm) gastrointestinal stromal tumor of the stomach based on analysis of 60 operated cases. Surgery 139:484–492
Huang CM, Chen QF, Lin JX, Lin M, Zheng CH, Li P, Xie JW, Wang JB, Lu J, Chen QY, Cao LL, Tu RH (2017) Can laparoscopic surgery be applied in gastric gastrointestinal stromal tumors located in unfavorable sites? A study based on the NCCN guidelines. Medicine (Baltimore) 96:e6535–e6542
Novitsky YW, Kercher KW, Sign RF, Heniford BT (2006) Long-term outcomes of laparoscopic resection of gastric gastrointestinal stromal tumors. Ann Surg 243:738–745
An W, Sun PB, Gao J, Jiang F, Liu F, Chen J, Wang D, Li ZS, Shi XG (2017) Endoscopic submucosal dissection for gastric gastrointestinal stromal tumors: a retrospective cohort study. Surg Endosc 31(11):4522–4531
He G, Wang J, Chen B, Xing X, Wang J, Chen J, He Y, Cui Y, Chen M (2016) Feasibility of endoscopic submucosal dissection for upper gastrointestinal submucosal tumors treatment and value of endoscopic ultrasonography in pre-operation assess and post-operation follow-up: a prospective study of 224 cases in a single medical center. Surg Endosc 30(10):4206–4213
Catalano F, Rodella L, Lombardo F, Silano M, Tomezzoli A, Fuini A, Di Cosmo MA, de Manzoni G, Trecca A (2013) Endoscopic submucosal dissection in the treatment of gastric submucosal tumors: results from a retrospective cohort study. Gastric Cancer 16(4):563–570
Yu C, Liao G, Fan C, Yu J, Nie X, Yang S, Bai J (2017) Long-term outcomes of endoscopic resection of gastric GISTs. Surg Endosc 31:4799–4804
Cho JW (2016) Current guidelines in the management of upper gastrointestinal subepithelial tumors. Clin Endosc 49:235–240
Herbella F, Tamasauskas I, Moura E (2016) Endogastric resection of gastrointestinal stromal tumor. J Vis Surg 2:161–163
He Z, Sun C, Zheng Z, Yu Q, Wang T, Chen X, Cao H, Liu W, Wang B (2013) Endoscopic submucosal dissection of large gastrointestinal stromal tumors in the esophagus and stomach. J Gastroenterol Hepatol 28:262–267
Li L, Wang F, Wu B, Wang Q, Wang C, Liu J (2013) Endoscopic submucosal dissection of gastric fundus subepithelial tumors originating from the muscularis propria. Exp Ther Med 6:391–395
Mangiavillano B, Viaggi P, Masci E (2010) Endoscopic closure of acute iatrogenic perforations during diagnostic and therapeutic endoscopy in the gastrointestinal tract using metallic clips: a literature review. J Dig Dis 11:12–18
Chen L, Zhang Q, Li FY, Yang L, Zhang DC, Wang LJ, Wang WZ, Li Z, Xu JH, He ZY, Xu KJ, Chen M, Xu H, Xu ZK (2018) Comparison of treatment outcomes between laparoscopic and endoscopic surgeries for relatively small gastric gastrointestinal stromal tumors. Surg Oncol 27:737–742
Ohta T, Ishihara R, Uedo N, Takeuchi Y, Nagai K, Matsui F, Kawada N, Yamashina T, Kanzaki H, Hanafusa M, Yamamoto S, Hanaoka N, Higashino K, Iishi H (2012) Factors predicting perforation during endoscopic submucosal dissection for gastric cancer. Gastrointest Endosc 75:1159–1165
Miettinen M, Lasota J (2006) Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol 23:70–83
Kiyozaki H, Saito M, Chiba H, Takata O, Rikiyama T (2014) Laparoscopic wedge resection of the stomach for gastrointestinal stromal tumor(GIST): non-touch lesion lifting method. Gastric Cancer 17:337–340
Nguyen SQ, Divino CM, Wang JL, Dikman SH (2006) Laparoscopic management of gastrointestinal stromal tumors. Surg Endosc 20:713–716
Berindoague R, Targarona EM, Feliu X, Artigas V, Balague C, Aldeano A, Lahoud A, Navine J, Fernandez-Sallent E, Trias M (2006) Laparoscopic resection of clinically suspected gastric stromal tumors. Surg Innov 13:231–237
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant nos. 81773117, 81771881, 81700576, and 81672446), the National Key Basic Research Program of China (Grant no. 2015CB352006), the National Clinical Key Specialty Construction Program (Grant no. [2011]170), the State’s Key Project of Research and Development Plan (Grant nos. 2017YFC0108300 and 2017YFC0108302), the Special Fund for Guangdong Province Public Research and Capacity Building (Grant no. 2014B020215002), the Natural Science Foundation of Guangdong Province (Grant no. 2015A030308006), the Guangzhou Industry University Research Cooperative Innovation Major Project (Grant no. 201704020062), the Special Fund from Clinical Research of Wu Jieping Medical Foundation (Grant no. 320.2710.1851), Clinical Research Startup Program of Southern Medical University by High-Level University Construction Funding of Guangdong Provincial Department of Education (Grant no. LC2016PY010), the High-Level Research Matching Foundation of Nanfang Hospital (Grant no. 2014067), the Scientific Research Foundation for High-Level Talents in Nanfang Hospital of Southern Medical University (Grant no. 201404280056), the Special Funds for the Cultivation of Guangdong College Students’ Scientific and Technological Innovation (Grant no. pdjh2019b0098), the Training Program for Undergraduate Innovation and Entrepreneurship (Grant nos. 201812121265, and 201812121039S), and the Scientific Enlightenment Plan of Southern Medical University (Grant no. B1000494).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Xiaoyu Dong, Weisheng Chen, Ziming Cui, Tao Chen, Xiumin Liu, Dexin Chen, Wei Jiang, Kai Li, Shumin Dong, Mingyuan Feng, Jixiang Zheng, Zhiming Li, Meiting Fu, Ying Lin, Jiaying Liao, Huijuan Le, and Jun Yan have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dong, X., Chen, W., Cui, Z. et al. Laparoscopic resection is better than endoscopic dissection for gastric gastrointestinal stromal tumor between 2 and 5 cm in size: a case-matched study in a gastrointestinal center. Surg Endosc 34, 5098–5106 (2020). https://doi.org/10.1007/s00464-019-07251-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07251-6