Abstract
Objectives
C-BLART (clip band ligation anti-reflux therapy) has been reported as a new alternative endoscopic treatment for refractory gastroesophageal reflux disease (GERD). This study evaluated the short-term efficacy of C-BLART for controlling GERD symptoms, esophageal acid exposure, esophagitis, and quality of life.
Methods
Patients with refractory GERD were recruited for a nonrandomized concurrent comparison, with 60 patients in the C-BLART with tailored PPI use group and 43 patients in the BID proton pump inhibitor (PPI) group. The primary outcomes were esophageal acid exposure and the lower esophageal sphincter (LES) pressure. The GERD-Q score, esophagitis grade, and adherence degree were also recorded. Crossover from the BID PPI group to the C-BLART with tailored PPI use group was allowed after 6 months.
Results
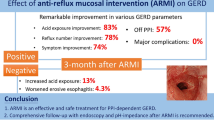
The LES pressure and GERD-Q score improved more in the C-BLART with tailored PPI use group (P < 0.001) after 6 months, with no significant difference in the decrease in esophagitis compared with the baseline endoscopic results (P = 0.268). Treatment with PPIs had been halted in 43% of the patients at 6 months after C-BLART. At 12 months after C-BLART, the DeMeester score showed a significant improvement compared with the baseline measurements (P = 0.025). The GERD-Q score and LES pressure did not significantly improve compared with the baseline values (P = 0.102, P = 0.184) in C-BLART with tailored PPI use group. At 6 to 12 months, n = 6 (10%) patients had undergone laparoscopic fundoplication to control their symptoms in all the patients after C-BLART.
Conclusion
C-BLART is a novel treatment for controlling refractory GERD symptoms, esophageal acid exposure, and LES pressure according to this short-term analysis, safely performed endoscopically to create an anti-reflux barrier with ligated bands. Despite improvements in DeMeester score, LES pressure, and GERD-Q scores in the C-BLART with tailored PPI use group, many patients continue to demonstrate objective evidence of GERD.




Similar content being viewed by others
References
Gyawali CP, Fass R (2017) Management of gastroesophageal reflux disease. Gastroenterology 154:302
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R (2006) The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 101:1900–1920 quiz 1943
El-Serag HB, Sweet S, Winchester CC, Dent J (2014) Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 63:871–880
Bredenoord AJ, Pandolfino JE, Smout AJ (2013) Gastro-oesophageal reflux disease. Lancet (London, England) 381:1933–1942
Azzam RS (2018) Are the persistent symptoms to proton pump inhibitor therapy due to refractory gastroesophageal reflux disease or to other disorders? Arq Gastroenterol 55(Suppl 1):85–91
Patti MG (2016) An evidence-based approach to the treatment of gastroesophageal reflux disease. JAMA Surg 151:73–78
Gerson LB, Robbins AS, Garber A, Hornberger J, Triadafilopoulos G (2000) A cost-effectiveness analysis of prescribing strategies in the management of gastroesophageal reflux disease. Am J Gastroenterol 95:395–407
Dean BB, Gano AD Jr, Knight K, Ofman JJ, Fass R (2004) Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin Gastroenterol Hepatol 2:656–664
Kuipers EJ, Lundell L, Klinkenberg-Knol EC, Havu N, Festen HP, Liedman B, Lamers CB, Jansen JB, Dalenback J, Snel P, Nelis GF, Meuwissen SG (1996) Atrophic gastritis and Helicobacter pylori infection in patients with reflux esophagitis treated with omeprazole or fundoplication. New Engl J Med 334:1018–1022
Lipham JC, DeMeester TR, Ganz RA, Bonavina L, Saino G, Dunn DH, Fockens P, Bemelman W (2012) The LINX(R) reflux management system: confirmed safety and efficacy now at 4 years. Surg Endosc 26:2944–2949
Anvari M, Allen C, Marshall J, Armstrong D, Goeree R, Ungar W, Goldsmith C (2006) A randomized controlled trial of laparoscopic nissen fundoplication versus proton pump inhibitors for treatment of patients with chronic gastroesophageal reflux disease: one-year follow-up. Surg Innov 13:238–249
Lundell L, Miettinen P, Myrvold HE, Pedersen SA, Liedman B, Hatlebakk JG, Julkonen R, Levander K, Carlsson J, Lamm M, Wiklund I (2001) Continued (5-year) followup of a randomized clinical study comparing antireflux surgery and omeprazole in gastroesophageal reflux disease. J Am Coll Surg 192:172–179 discussion 179-181
Spechler SJ, Lee E, Ahnen D, Goyal RK, Hirano I, Ramirez F, Raufman JP, Sampliner R, Schnell T, Sontag S, Vlahcevic ZR, Young R, Williford W (2001) Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: follow-up of a randomized controlled trial. JAMA 285:2331–2338
Frazzoni M, Piccoli M, Conigliaro R, Frazzoni L, Melotti G (2014) Laparoscopic fundoplication for gastroesophageal reflux disease. World J Gastroenterol 20:14272–14279
Yates RB, Oelschlager BK (2015) Surgical treatment of gastroesophageal reflux disease. Surg clin N Am 95:527–553
Enqiang Linghu YW, Wang Xiaoxiao (2013) Endoscopic cardial coarctation in the treatment of gastroesophageal reflux disease: a case report. Chin J Endosc surg (Electronic Edition) 6:468–469
Li X, Zhang XB, Hu HQ, Li HK, Wang XX, Linghu EQ (2017) Effect and safety of peroral endoscopic cardial constriction for gastroesophageal reflux disease. Chin Med J 130:1749–1750
Jones R, Junghard O, Dent J, Vakil N, Halling K, Wernersson B, Lind T (2009) Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 30:1030–1038
Katz PO, Gerson LB, Vela MF (2013) Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 108:308–328 quiz 329
Labenz J, Malfertheiner P (2005) Treatment of uncomplicated reflux disease. World J Gastroenterol 11:4291–4299
Shaheen NJ, Denison H, Bjorck K, Karlsson M, Silberg DG (2013) Efficacy and safety of lesogaberan in gastro-oesophageal reflux disease: a randomised controlled trial. Gut 62:1248–1255
Vela MF, Camacho-Lobato L, Srinivasan R, Tutuian R, Katz PO, Castell DO (2001) Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology 120:1599–1606
Galmiche JP, Hatlebakk J, Attwood S, Ell C, Fiocca R, Eklund S, Langstrom G, Lind T, Lundell L (2011) Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA 305:1969–1977
Lundell L, Attwood S, Ell C, Fiocca R, Galmiche JP, Hatlebakk J, Lind T, Junghard O (2008) Comparing laparoscopic antireflux surgery with esomeprazole in the management of patients with chronic gastro-oesophageal reflux disease: a 3-year interim analysis of the LOTUS trial. Gut 57:1207–1213
Mehta S, Bennett J, Mahon D, Rhodes M (2006) Prospective trial of laparoscopic nissen fundoplication versus proton pump inhibitor therapy for gastroesophageal reflux disease: seven-year follow-up. J Gastrointest Surg 10:1312–1316 discussion 1316-1317
Bredenoord AJ, Draaisma WA, Weusten BL, Gooszen HG, Smout AJ (2008) Mechanisms of acid, weakly acidic and gas reflux after anti-reflux surgery. Gut 57:161–166
Staehelin A, Zingg U, Devitt PG, Esterman AJ, Smith L, Jamieson GG, Watson DI (2014) Preoperative factors predicting clinical outcome following laparoscopic fundoplication. World J Surg 38:1431–1443
Oor JE, Roks DJ, Broeders JA, Hazebroek EJ, Gooszen HG (2017) Seventeen-year outcome of a randomized clinical trial comparing laparoscopic and conventional nissen fundoplication: a plea for patient counseling and clarification. Ann Surg 266:23–28
Patti MG, Allaix ME, Fisichella PM (2015) Analysis of the causes of failed antireflux surgery and the principles of treatment: a review. JAMA Surg 150:585–590
Fass R, Cahn F, Scotti DJ, Gregory DA (2017) Systematic review and meta-analysis of controlled and prospective cohort efficacy studies of endoscopic radiofrequency for treatment of gastroesophageal reflux disease. Surg Endosc 31:4865–4882
Richter J, Kumar A, Lipka S, Miladinovic B, Velanovich V (2018) Efficacy of laparoscopic nissen fundoplication vs transoral incisionless fundoplication or proton pump inhibitors in patients with gastroesophageal reflux disease: a systematic review and network meta-analysis. Gastroenterology 154:1298
Inoue H, Ito H, Ikeda H, Sato C, Sato H, Phalanusitthepha C, Hayee B, Eleftheriadis N, Kudo SE (2014) Anti-reflux mucosectomy for gastroesophageal reflux disease in the absence of hiatus hernia: a pilot study. Ann Gastroenterol 27:346–351
Acknowledgements
This work was supported by grants from the National Key R&D Program of China (2016YFC1303601). No other funding organization played a role in the design or conduct of the study, the collection, management, analysis, or interpretation of the data, or the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs.Liu, Chai, Zhai, Zou, Feng, Li, Li, Zhang, Wang, Wang, and Linghu have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, S., Chai, N., Zhai, Y. et al. New treatment method for refractory gastroesophageal reflux disease (GERD): C-BLART (clip band ligation anti-reflux therapy)—a short-term study. Surg Endosc 34, 4516–4524 (2020). https://doi.org/10.1007/s00464-019-07238-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07238-3