Abstract
Background
Laparoscopic surgery for colorectal cancer has been shown in clinical trials to be effective regarding short-term outcomes and oncologically safe. Health economic analyses have been performed early in the learning curve when adoption of laparoscopic surgery was not extensive. This cost-effectiveness analysis evaluates laparoscopic versus open colorectal cancer surgery in Swedish routine care.
Methods
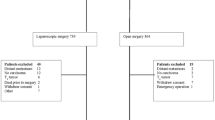
In this national retrospective cohort study, data were retrieved from the Swedish ColoRectal Cancer Registry. Clinical effectiveness, resource use and unit costs were derived from this and other sources with nationwide coverage. The study period was 2013 and 2014 with 1 year follow-up. Exclusion criterion comprised cT4-tumors. Clinical effectiveness was estimated in a composite endpoint of all-cause resource-consuming events in inpatient care, readmissions and deaths up to 90 days postoperatively. Up to 1 year, events predefined as related to the primary surgery were included. Costs included resource-consuming events, readmissions and sick leave and were estimated for both the society and healthcare. Multivariable regression analyses were used to adjust for differences in baseline characteristics between the groups.
Results
After exclusion of cT4 tumors, the cohort included 7707 patients who underwent colorectal cancer surgery: 6060 patients in the open surgery group and 1647 patients in the laparoscopic group. The mean adjusted difference in clinical effectiveness between laparoscopic and open colorectal cancer surgery was 0.23 events (95% CI 0.12 to 0.33). Mean adjusted differences in costs (open minus laparoscopic surgery) were $4504 (95% CI 2257 to 6799) and $4480 (95% CI 2739 to 6203) for the societal and the healthcare perspective respectively. In both categories, resource consuming events in inpatient care were the main driver of the results.
Conclusion
In a national cohort, laparoscopic colorectal cancer surgery was associated with both superior outcomes for clinical effectiveness and cost versus open surgery.
Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–386
Clinical Outcomes of Surgical Therapy Study G, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM, Group COcLoORS (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G, Clinical Outcomes of Surgical Therapy Study G (2002) Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. JAMA 287:321–328
Janson M, Lindholm E, Anderberg B, Haglind E (2007) Randomized trial of health-related quality of life after open and laparoscopic surgery for colon cancer. Surg Endosc 21:747–753
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E, Group CIS (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, Bonjer HJ, Group COcLoORIS (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J, Investigators AL (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314:1356–1363
Bhama AR, Obias V, Welch KB, Vandewarker JF, Cleary RK (2016) A comparison of laparoscopic and robotic colorectal surgery outcomes using the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database. Surg Endosc 30:1576–1584
Jayne D, Pigazzi A, Marshall H, Croft J, Corrigan N, Copeland J, Quirke P, West N, Rautio T, Thomassen N, Tilney H, Gudgeon M, Bianchi PP, Edlin R, Hulme C, Brown J (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer: the ROLARR randomized clinical trial. JAMA 318:1569–1580
Son HJ, Lee HY, Park JW, Choi HS, Jeong SY, Oh JH (2013) Cost-comparison of laparoscopic and open surgery for mid or low rectal cancer after preoperative chemoradiotherapy: data from a randomized controlled trial. World J Surg 37:214–219
Franks PJ, Bosanquet N, Thorpe H, Brown JM, Copeland J, Smith AM, Quirke P, Guillou PJ, Participants Ct (2006) Short-term costs of conventional vs laparoscopic assisted surgery in patients with colorectal cancer (MRC CLASICC trial). Br J Cancer 95(1):6–12
Janson M, Bjorholt I, Carlsson P, Haglind E, Henriksson M, Lindholm E, Anderberg B (2004) Randomized clinical trial of the costs of open and laparoscopic surgery for colonic cancer. Br J Surg 91:409–417
Gehrman J, Bjorholt I, Angenete E, Andersson J, Bonjer J, Haglind E (2017) Health economic analysis of costs of laparoscopic and open surgery for rectal cancer within a randomized trial (COLOR II). Surg Endosc 31:1225–1234
Jordan J, Dowson H, Gage H, Jackson D, Rockall T (2014) Laparoscopic versus open colorectal resection for cancer and polyps: a cost-effectiveness study. Clinicoecon Outcomes Res 6:415–422
Thompson BS, Coory MD, Gordon LG, Lumley JW (2014) Cost savings for elective laparoscopic resection compared with open resection for colorectal cancer in a region of high uptake. Surg Endosc 28:1515–1521
Braga M, Vignali A, Zuliani W, Frasson M, Di Serio C, Di Carlo V (2005) Laparoscopic versus open colorectal surgery: cost-benefit analysis in a single-center randomized trial. Ann Surg 242:890–895 Discussion 895-896
Kodeda K, Nathanaelsson L, Jung B, Olsson H, Jestin P, Sjovall A, Glimelius B, Pahlman L, Syk I (2013) Population-based data from the Swedish Colon Cancer Registry. Br J Surg 100:1100–1107
Pahlman L, Bohe M, Cedermark B, Dahlberg M, Lindmark G, Sjodahl R, Ojerskog B, Damber L, Johansson R (2007) The Swedish rectal cancer registry. Br J Surg 94:1285–1292
Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL (2005) Methods for the economic evaluation of health care programmes, 3rd edn. Oxford University Press, Oxford
Glick H, Doshi JA, Sonnad SS, Polsky D (2014) Economic evaluation in clinical trials. Oxford University Press, Oxford
Bang H, Tsiatis AA (2000) Estimating medical costs with censored data. Biometrika 87:329–343
OECD (2016) Purchasing power parities. https://data.oecd.org/conversion/purchasing-power-parities-ppp.htm. Accessed 24 Mar 2019
Drummond M, McGuire A (2001) Economic evaluation in health care: merging theory with practice. Oxford University Press, Oxford
Manning WG, Mullahy J (2001) Estimating log models: to transform or not to transform? J Health Econ 20:461–494
Pregibon D (1980) Goodness of Link Tests for Generalized Linear Models. J R Stat Soc Ser C Appl Stat 29:15–23 (14)
Hosmer DW Jr, Lemeshow S, Sturdivant RX (2013) Applied logistic regression. Wiley, Hoboken, NJ
Copas JB (1997) Using regression models for prediction: shrinkage and regression to the mean. Stat Methods Med Res 6:167–183
Barber JA, Thompson SG (2000) Analysis of cost data in randomized trials: an application of the non-parametric bootstrap. Stat Med 19:3219–3236
Sheetz KH, Norton EC, Regenbogen SE, Dimick JB (2017) An Instrumental Variable Analysis Comparing Medicare Expenditures for Laparoscopic vs Open Colectomy. JAMA Surg 152:921–929
Keller DS, Delaney CP, Hashemi L, Haas EM (2016) A national evaluation of clinical and economic outcomes in open versus laparoscopic colorectal surgery. Surg Endosc 30:4220–4228
Govaert JA, Fiocco M, van Dijk WA, Kolfschoten NE, Prins HA, Dekker JT, Tollenaar RA, Tanis PJ, Wouters MW (2016) Multicenter stratified comparison of hospital costs between laparoscopic and open colorectal cancer resections: influence of tumor location and operative risk. Ann Surg 266:1021–1028
DCCG (2010) Landsdækkende database for kræft i tyktarm og endetarm—Årsrapport 2009. https://dccg.dk/wp-content/uploads/2017/10/Aarsrapport_2009.pdf. Accessed 24 Mar 2019
Thompson BS, Coory MD, Lumley JW (2011) National trends in the uptake of laparoscopic resection for colorectal cancer, 2000-2008. Med J Aust 194:443–447
Schwab KE, Dowson HM, Van Dellen J, Marks CG, Rockall TA (2009) The uptake of laparoscopic colorectal surgery in Great Britain and Ireland: a questionnaire survey of consultant members of the ACPGBI. Colorectal Dis 11:318–322
Bartels SA, Vlug MS, Hollmann MW, Dijkgraaf MG, Ubbink DT, Cense HA, van Wagensveld BA, Engel AF, Gerhards MF, Bemelman WA, Collaborative LSG (2014) Small bowel obstruction, incisional hernia and survival after laparoscopic and open colonic resection (LAFA study). Br J Surg 101:1153–1159
Cerdán Santacruz C, Frasson M, Flor-Lorente B, Ramos Rodríguez JL, Trallero Anoro M, Millán Scheiding M, Maseda Díaz O, Dujovne Lindenbaum P, Monzón Abad A, García-Granero Ximenez E (2017) Laparoscopy may decrease morbidity and length of stay after elective colon cancer resection, especially in frail patients: results from an observational real-life study. Surg Endosc 31:5032–5042
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, Heurgren M, Olausson PO (2011) External review and validation of the Swedish national inpatient register. BMC Public Health 11:450
Kodeda K, Johansson R, Zar N, Birgisson H, Dahlberg M, Skullman S, Lindmark G, Glimelius B, Pahlman L, Martling A (2015) Time trends, improvements and national auditing of rectal cancer management over an 18-year period. Colorectal Dis 17:O168–179
Acknowledgements
Open access funding provided by University of Gothenburg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Eva Angenete reports grant from Sahlgrenska University Hospital, ALF Agreement concerning research and education of doctors (ALFGBG-716581). Ingela Björholt and Eva Lesén reports remuneration for work paid to employer (PharmaLex Sweden AB) from University of Gothenburg, during the conduct of the study. Eva Haglind reports Grants from Swedish Cancer Society (2016-362), grants from ALF-Gbg (4307771) during the conduct of the study. Jacob Gehrman have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gehrman, J., Angenete, E., Björholt, I. et al. Cost-effectiveness analysis of laparoscopic and open surgery in routine Swedish care for colorectal cancer. Surg Endosc 34, 4403–4412 (2020). https://doi.org/10.1007/s00464-019-07214-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07214-x