Abstract
Objective
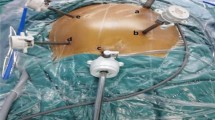
To explore the feasibility and application value of a “caudal-to-cranial” plus “artery first” technique with beyond D3 lymph node dissection on the right midline of the superior mesenteric artery (SMA) for the treatment of right colon cancer
Methods
Clinical data consisting of 168 right colon cancer cases under going laparoscopic D3 radical resection, including 84 cases of “caudal-to-cranial” plus “artery first” technique with beyond D3 lymph node dissection on the right midline of the SMA (CC + SMA group) and 84 cases of conventional medial approach plus dissection around the superior mesenteric vein (MA + SMV group), from January 2017 to March 2018 were retrospectively analyzed. For CC + SMA group, our surgical method was to isolate the mesocolon using a caudal-to-cranial pathway and ligate blood vessels along the midline of the SMA.
Results
The baseline data was not significantly different between the two groups (all p > 0.05). The mean operation time and intraoperative blood loss in the CC + SMA and the MA + SMV groups were 170.04 ± 43.10 versus 172.33 ± 41.84 min and 91.07 ± 55.12 versus 77.38 ± 40.21 ml, respectively, which has no significant difference (p > 0.05). The mean number of total and positive harvested lymph nodes in the two groups were 29.44 ± 5.90 versus 26.21 ± 6.64 (p < 0.05) and 2.57 ± 1.93 versus 2.51 ± 1.05, respectively (p > 0.05). Compared with the MA + SMV group, there was no significant difference in total postoperative complication rate in the CC + SMA group. The time to pull out drainage tube in the CC + SMA group was longer than MA + SMV group (4.05 ± 1.79 versus 3.38 ± 1.99 day; p = 0.022).
Conclusion
It is safe and feasible for the “caudal-to-cranial” plus “artery first” technique with beyond D3 lymph node dissection on the right midline of the SMA in right colon cancer. It may have some advantages in the number of lymph nodes dissection, and the long-term prognosis remains to be expected.








Similar content being viewed by others
References
Clinical Outcomes of Surgical Therapy Study Group, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, Beart RW Jr, Hellinger M, Flanagan R Jr, Peters W, Ota D (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350(20):2050–2059
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM, MRC CLASICC trial group (2005) Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRCCLASICC trial): multicentre, randomised controlled trial. Lancet 365(9472):1718–1726
Hewett PJ, Allardyce RA, Bagshaw PF, Frampton CM, Frizelle FA, Rieger NA et al (2008) Short-term outcomes of the Australasian randomized clinical study comparing laparoscopic and conventional open surgical treatments for colon cancer: the ALCCaS trial. Ann Surg 248(5):728–738
Hazebroek EJ (2002) COLOR: a randomized clinical trial comparing laparoscopic and open resection for colon cancer. Surg Endosc 16(6):949–953
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal Dis 11:354–364 Discussion 64–65
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P (2010) Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 28:272–278
West NP, Kobayashi H, Takahashi K et al (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30:1763–1769
West NP, Morris EJ, Rotimi O, Cairns A, Finan PJ, Quirke P (2008) Pathology grading of colon cancer surgical resection and its association with survival: a retrospective observational study. Lancet Oncol 9:857–865
Higuchi T, Sugihara K (2010) Complete mesocolic excision (CME) with central vascular ligation (CLV) as standardised surgical technique for colonic cancer: a Japanese multicentre study. Dis Colon Rectum 53:abstr176
Li H, He Y, Lin Z, Xiong W, Diao D, Wang W, Wan J, Zou L (2016) Laparoscopic caudal-to-cranial approach for radical lymph node dissection in right hemicolectomy. Langenbecks Arch Surg 401(5):741–746
Turnbull RB Jr, Kyle K, Watson FR, Spratt J (1967) Cancer of the colon: the influence of the no-touch isolation technique on survival rates. Ann Surg 166:420–425
Søndenaa K, Quirke P, Hohenberger W, Sugihara K, Kobayashi H, Kessler H, Brown G, Tudyka V, D’Hoore A, Kennedy RH, West NP, Kim SH, Heald R, Storli KE, Nesbakken A, Moran B (2014) The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery: proceedings of a consensus conference. Int J Colorectal Dis 29(4):419–428
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Japanese Society for Cancer of the Colon and Rectum et al (2012) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol 17(1):1–29
Nesgaard JM, Stimec BV, Soulie P, Edwin B, Bakka A, Ignjatovic D (2018) Defining minimal clearances for adequate lymphatic resection relevant to right colectomy for cancer: a post-mortem study. Surg Endosc 32(9):3806–3812
Benz SR, Tannapfel A, Tam Y, Stricker I (2015) Complete mesocolic excision for right-sided colon cancer the role of central lymph nodes. Zentralbl Chir 140(4):449–452
Zhao LY, Liu H, Wang YN, Deng HJ, Xue Q, Li GX (2014) Techniques and feasibility of laparoscopic extended right hemicolectomy with D3 lymphadenectomy. World J Gastroenterol 20(30):10531–10536
Kanemitsu Y, Komori K, Kimura K, Kato T (2013) D3 Lymph Node Dissection in Right Hemicolectomy with a No-touch Isolation Technique in Patients With Colon Cancer. Dis Colon Rectum 56(7):815–824
Benz S, Tam Y, Tannapfel A, Stricker I (2016) The uncinate process first approach: a novel technique for laparoscopic right hemicolectomy with complete mesocolic excision. SurgEndosc 30(5):1930–1937
Feng B, Sun J, Ling TL, Lu AG, Wang ML, Chen XY, Ma JJ, Li JW, Zang L, Han DP, Zheng MH (2012) Laparoscopic complete mesocolic excision (CME) with medial access for right-hemi colon cancer: feasibility and technical strategies. Surg Endosc 26:3669–3675
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications a new proposal with evaluation in a cohort of 6336 patients and Results of a survey. Ann Surg 240(2):205–213
Acar HI, Comert A, Avsar A, Celik S, Kuzu MA (2014) Dynamic article: surgical anatomical planes for complete mesocolic excision and applied vascular anatomy of the right colon. Dis Colon Rectum 57(10):1169–1175
Ogino T, Takemasa I, Horitsugi G, Furuyashiki M, Ohta K, UemuraM Nishimura J, Hata T, Mizushima T, Yamamoto H, Doki Y, Mori M (2014) Preoperative evaluation of venous anatomy in laparoscopic complete mesocolic excision for right colon cancer. Ann Surg Oncol 21(Suppl 3):S429–S435
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA (2007) Lymph node evaluation and survival after curative resection ofcolon cancer: systematic review. J Natl Cancer Inst 9:433–441
Vather R, Sammour T, Kahokehr A, Connolly AB, Hill AG (2009) Lymph node evaluation and long-term survival in stage II and stage III colon cancer: a national study. Ann Surg Oncol 16:585–593
Zhu DJ, Chen XW, OuYang MZ, Lu Y (2016) Three surgical planes identified in laparoscopic complete mesocolic excision for right-sided colon cancer. World J Surg Oncol 14(1):7
Nakajima K, Inomata M, Akagi T, Etoh T, Sugihara K, Watanabe M, Yamamoto S, Katayama H, Moriya Y, Kitano S (2014) Quality control by photo documentation for evaluation of laparoscopic and open colectomy with D3 resection for stage II/III colorectal cancer: Japan Clinical Oncology Group Study JCOG 0404. Jpn J Clin Oncol 44(9):799–806
Tsai HL, Lu CY, Hsieh JS, Wu DC, Jan CM, Chai CY, Chu KS, Chan HM, Wang JY (2007) The prognostic significance of total lymph node harvest in patients with T2-4N0M0 colorectal cancer. J Gastrointest Surg 11:660–665
Rosenberg R, Engel J, Bruns C, Heitland W, Hermes N, Jauch KW, Kopp R, Pütterich E, Ruppert R, Schuster T, Friess H, Hölzel D (2010) The prognostic value of lymph node ratio in a population based collective of colorectal cancer patients. Ann Surg 251(6):1070–1078
Hasegawa S, Kawamura J, Nagayama S, Nomura A, Kondo K, Sakai Y (2007) Medially approached radical lymph node dissection along the surgical trunk for advanced right-sided colon cancers. Surg Endosc 21(9):1657
Kawahara H, Hirai K, Watanabe K, Kashiwagi H, Yamazaki Y, Yanaga K (2005) New approach for laparoscopic surgery of the right colon. Dig Surg 22:50
Tepper JE, O’Connell MJ, Niedzwiecki D, Hollis D, Compton C, Benson AB III, Cummings B, Gunderson L, Macdonald JS, Mayer RJ (2001) Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol 19:157–163
Barnes JP (1952) Physiologic resection of the right colon. Surg Gynecol Obstet 94:722–726
Wiggers T, Jeekel J, Arends JW, Brinkhorst AP, Kluck HM, Luyk CI, Munting JD, Povel JA, Rutten AP, Volovics A (1988) No-touch isolation technique in colon cancer: a controlled prospective trial. Br J Surg 75:409–415
Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, Pique JM (2008) The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg 248(1):1–7
Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Hellinger M, Flanagan R, Peters W, Nelson H (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study grouptrial. Ann Surg 246:655–662
Adamina M, Manwaring ML, Park KJ, Delaney CP (2012) Laparoscopic complete mesocolic excision for right colon cancer. Surg Endosc 26(10):2976–2980
Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K, Matsumoto J (2010) Postoperative bowel function and nutritional status following distal pancreatectomy with en-bloc celiac axis resection. Dig Surg 27(3):212–216
Hirano S, Kondo S, Hara T, Ambo Y, Tanaka E, Shichinohe T, Suzuki O, Hazama K (2007) Distal pancreatectomy with en bloc celiac axis resection for locally advanced pancreatic body cancer: long-term results. Ann Surg 246(1):46–51
Acknowledgements
Our authors deeply appreciate the contributions of all the coworkers and friends to this study and, furthermore, appreciate the editors and reviewers for their help with the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Xiaojiang Yi, Hongming Li, Xinquan Lu, Jin Wan, and Dechang Diao have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yi, X., Li, H., Lu, X. et al. “Caudal-to-cranial” plus “artery first” technique with beyond D3 lymph node dissection on the right midline of the superior mesenteric artery for the treatment of right colon cancer: is it more in line with the principle of oncology?. Surg Endosc 34, 4089–4100 (2020). https://doi.org/10.1007/s00464-019-07171-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07171-5