Abstract
Background/aim
Distal pancreatectomy (DP) accounts for 25% of all pancreatic resections. Complications following DP occur in around 40% of the cases. Our aim is to analyze short-term surgical outcomes of DP based on whether the indication for resection was benign or malignant pathology, as well as the effect of the surgical approach, open versus laparoscopic on morbidity and mortality.
Methods
We studied all patients undergoing DP from the National Surgery Quality Improvement Program (NSQIP) targeted pancreatectomy participant use file from 2014 to 2016. The patients were divided into 2 groups, those who underwent DP for benign diseases (DP-B) and those who underwent DP for malignant diseases (DP-M). We performed multivariate logistic regression to evaluate the association between benign or malignant distal pancreatectomies and 30-day outcomes. We included clinically and/or statistically significant confounders into the models. We also conducted the same analysis in the subgroups of open and laparoscopic DP.
Results
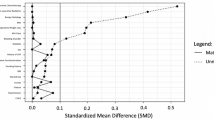
Three thousand five hundred and seventy-nine patients underwent distal pancreatectomy. The most common indication for surgery was malignant disease in 1894 (53%). Thirty-day mortality occurred in 0.4% of DP-B compared to 1.3% DP-M. On multivariate analysis, no significant difference was found in mortality or in the risk of pancreatic fistula between the 2 groups. Bleeding (p = 0.002) and composite morbidity (p = 0.01) were significantly higher in the DP-M group. Among composite morbidities, thromboembolism was significantly associated with DP-M (OR 2.1, p = 0.0004) only when performed with an open approach.
Conclusion
DP-M is associated with a significantly higher risk of post-operative bleeding, thromboembolism, and sepsis compared to DP-B but no significant increase in mortality. When further analyzing the impact of the operative approach on morbidity, there was an increased rate of post-operative thromboembolic in the DP-M group when the surgery was performed in an open manner and this increased risk was no longer statistically significant if the DP-M was performed using a minimally invasive approach.
Similar content being viewed by others
References
Büchler MW, Wagner M, Schmied BM, Uhl W, Friess H, Z’graggen K (2003) Changes in morbidity after pancreatic resection: toward the end of completion pancreatectomy. Arch Surg 138:1310–1314
Cameron JL, Pitt HA, Yeo CJ, Lillemoe KD, Kaufman HS, Coleman J (1993) One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg 217:430
van Heek NT, Kuhlmann KF, Scholten RJ, de Castro SM, Busch OR, van Gulik TM, Obertop H, Gouma DJ (2005) Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in the Netherlands. Ann Surg 242:781
Kooby DA, Gillespie T, Bentrem D, Nakeeb A, Merchant NB, Parikh AA, Martin RC, Scoggins CR, Ahmad S, Kim HJ (2008) Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann Surg 248:438–446
Lyman GH (2011) Venous thromboembolism in the patient with cancer: focus on burden of disease and benefits of thromboprophylaxis. Cancer 117:1334–1349
Tzeng C-WD, Katz MH, Lee JE, Fleming JB, Pisters PW, Vauthey J-N, Aloia TA (2014) Predicting the risks of venous thromboembolism versus post-pancreatectomy haemorrhage: analysis of 13 771 NSQIP patients. HPB 16:373–383
Sulpice L, Farges O, Goutte N, Bendersky N, Dokmak S, Sauvanet A, Delpero JR (2015) Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: time for a randomized controlled trial? Results of an all-inclusive national observational study. Ann Surg 262:868–873 discussion 873–864
Plotkin A, Ceppa EP, Zarzaur BL, Kilbane EM, Riall TS, Pitt HA (2017) Reduced morbidity with minimally invasive distal pancreatectomy for pancreatic adenocarcinoma. HPB 19:279–285
Zhang M, Fang R, Mou Y, Chen R, Xu X, Zhang R, Yan J, Jin W, Ajoodhea H (2015) LDP vs ODP for pancreatic adenocarcinoma: a case matched study from a single-institution. BMC Gastroenterol 15:182
de Rooij T, Klompmaker S, Hilal MA, Kendrick ML, Busch OR, Besselink MG (2016) Laparoscopic pancreatic surgery for benign and malignant disease. Nat Rev Gastroenterol Hepatol 13:227
Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA Jr, Fink AS, Mentzer RM Jr, Steeger JE (2007) The patient safety in surgery study: background, study design, and patient populations. J Am Coll Surg 204:1089–1102
Fink AS, Campbell DA Jr, Mentzer RM Jr, Henderson WG, Daley J, Bannister J, Hur K, Khuri SF (2002) The National Surgical Quality Improvement Program in non-veterans administration hospitals: initial demonstration of feasibility. Ann Surg 236:344–353 discussion 353–344
Shiloach M, Frencher SK, Steeger JE, Rowell KS, Bartzokis K, Tomeh MG, Richards KE, Ko CY, Hall BL (2010) Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 210:6–16
Solcia E, Capella C, Klppel G (1997) Tumors of the Pancreas: AFIP Atlas of Tumor Pathology, 3rd series, fascicle 20. Armed Forces Institute of Pathology, Washington, pp 14–18
Adsay N, Fukushima N, Furukawa T, Hruban R, Klimstra D, Klöppel G, Offerhaus G, Pitman M, Shimizu M, Zamboni G (2010) WHO classification of tumours of the digestive system. Intraductal neoplasm of the pancreas. WHO, Lyon, p 304
Pelzer U, Opitz B, Deutschinoff G, Stauch M, Reitzig PC, Hahnfeld S, Müller L, Grunewald M, Stieler JM, Sinn M (2015) Efficacy of prophylactic low-molecular weight heparin for ambulatory patients with advanced pancreatic cancer: outcomes from the CONKO-004 trial. J Clin Oncol 33:2028–2034
Ay C, Dunkler D, Marosi C, Chiriac A-L, Vormittag R, Simanek R, Quehenberger P, Zielinski C, Pabinger I (2010) Prediction of venous thromboembolism in cancer patients. Blood 116:5377–5382
Otten H-MM, Mathijssen J, ten Cate H, Soesan M, Inghels M, Richel DJ, Prins MH (2004) Symptomatic venous thromboembolism in cancer patients treated with chemotherapy: an underestimated phenomenon. Arch Intern Med 164:190–194
van Es N, Di Nisio M, Cesarman G, Kleinjan A, Otten H-M, Mahé I, Wilts IT, Twint DC, Porreca E, Arrieta O (2017) Comparison of risk prediction scores for venous thromboembolism in cancer patients: a prospective cohort study. Haematologica 102:1494–1501
Ansari D, Ansari D, Andersson R, Andrén-Sandberg Å (2015) Pancreatic cancer and thromboembolic disease, 150 years after Trousseau. Hepatobiliary Surg Nutr 4:325
Butler JR, Eckert GJ, Zyromski NJ, Leonardi MJ, Lillemoe KD, Howard TJ (2011) Natural history of pancreatitis-induced splenic vein thrombosis: a systematic review and meta-analysis of its incidence and rate of gastrointestinal bleeding. HPB 13:839–845
Pulvirenti A, Pea A, De Pastena M, Marchegiani G, Salvia R, Bassi C (2018) Postoperative management in patients undergoing major pancreatic resections. surgery for pancreatic and periampullary cancer. Springer, New York, pp 239–245
De Martino RR, Goodney PP, Spangler EL, Wallaert JB, Corriere MA, Rzucidlo EM, Walsh DB, Stone DH (2012) Variation in thromboembolic complications among patients undergoing commonly performed cancer operations. J Vasc Surg 55:1035–1040.e1034
Nakamura M, Wakabayashi G, Miyasaka Y, Tanaka M, Morikawa T, Unno M, Tajima H, Kumamoto Y, Satoi S, Kwon M, Toyama H, Ku Y, Yoshitomi H, Nara S, Shimada K, Yokoyama T, Miyagawa S, Toyama Y, Yanaga K, Fujii T, Kodera Y, Tomiyama Y, Miyata H, Takahara T, Beppu T, Yamaue H, Miyazaki M, Takada T (2015) Multicenter comparative study of laparoscopic and open distal pancreatectomy using propensity score-matching. J Hepato Biliary Pancreat Sci 22:731–736
Jin T, Altaf K, Xiong JJ, Huang W, Javed MA, Mai G, Liu XB, Hu WM, Xia Q (2012) A systematic review and meta-analysis of studies comparing laparoscopic and open distal pancreatectomy. HPB 14:711–724
van Hilst J, de Rooij T, Klompmaker S, Rawashdeh M, Aleotti F, Al-Sarireh B, Alseidi A, Ateeb Z, Balzano G, Berrevoet F (2019) Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a Pan-European Propensity Score Matched Study. Ann Surg 269:10–17
de Rooij T, van Hilst J, van Santvoort H, Boerma D, van den Boezem P, Daams F, van Dam R, Dejong C, van Duyn E, Dijkgraaf M (2019) Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg 269:2–9
Funding
Not funded.
Author information
Authors and Affiliations
Contributions
All the authors met all 4 criteria as per the ICMJE.
Corresponding authors
Ethics declarations
Disclosures
Fady Daniel, Hani Tamim, Mohammad Hosni, Aurelie Mailhac, Mohamad Khalife, Faek Jamali, and Walid Faraj have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Daniel, F.E., Tamim, H.M., Hosni, M.N. et al. Short-term surgical morbidity and mortality of distal pancreatectomy performed for benign versus malignant diseases: a NSQIP analysis. Surg Endosc 34, 3927–3935 (2020). https://doi.org/10.1007/s00464-019-07163-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07163-5