Abstract
Background
Liver is a common metastatic site not only of colorectal but of non-colorectal neoplasms, as well. However, resection of non-colorectal liver metastases (NCRLMs) remains controversial. The aim of this retrospective study was to analyze the short- and long-term outcomes of patients undergoing laparoscopic liver resection (LLR) for NCRLMs.
Methods
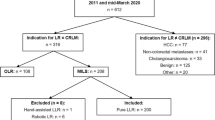
From a prospectively maintained database between 2000 and 2018, patients undergoing LLR for colorectal liver metastases (CRLMs) and NCRLMs were selected. Clinicopathologic, operative, short- and long-term outcome data were collected, analyzed, and compared among patients with CRLMs and NCRLMs.
Results
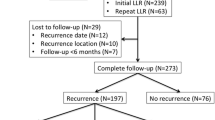
The primary tumor was colorectal in 354 (82.1%), neuroendocrine in 21 (4.9%), and non-colorectal, non-neuroendocrine in the remaining 56 (13%) patients. Major postoperative morbidities were 12.7%, 19%, and 3.6%, respectively (p = 0.001), whereas the mortality was 0.6% for patients with CRLMs and zero for patients with NCRLMs. The rate of R1 surgical margin was comparable (p = 0.432) among groups. According to the survival analysis, 3- and 5-year recurrence-free survival (RFS) rates were 76.1% and 64.3% in the CRLM group, 57.1% and 42.3% in the neuroendocrine liver metastase (NELM) group, 33% and 20.8% in the non-colorectal, non-neuroendocrine liver metastase (NCRNNELM) group (p = 0.001), respectively. Three- and 5-year overall survival (OS) rates were 88.3% and 82.7% in the CRLM group, 85.7% and 70.6% in the NELM group, 71.4% and 52.9% in the NCRNNELM group (p = 0.001), respectively. In total, 113 out of 354 (31.9%) patients with CRLMs, 2 out of 21(9.5%) with NELMs, and 8 out of 56 (14.3%) patients with NCRNNELMs underwent repeat LLR for recurrent metastatic tumors.
Conclusion
LLR is safe and feasible in the context of a multimodal management where an aggressive surgical approach, necessitating even complex procedures for bilobar multifocal metastases and repeat hepatectomy for recurrences, is the mainstay and may be of benefit in the long-term survival, in selected patients with NCRNNELMs.


Similar content being viewed by others
Abbreviations
- CRLMs:
-
Colorectal liver metastases
- NCRLMs:
-
Non-colorectal liver metastases
- NELMs:
-
Neuroendocrine liver metastases
- NETs:
-
Neuroendocrine tumors
- NCRNNELMs:
-
Non-colorectal non-neuroendocrine liver metastases
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- RFA:
-
Radiofrequency ablation
- LLR:
-
Laparoscopic liver resection
- EHD:
-
Extrahepatic disease
- CT-scan:
-
Computerized tomography scanner
- MRI:
-
Magnetic resonance imaging
- PVE:
-
Portal vein embolization
- FLR:
-
Future liver remnant
- GEP:
-
Gastroenteropancreatic
References
Kemeny N (2010) The management of resectable and unresectable liver metastases from colorectal cancer. Curr Opin Oncol 22:364–373
Lupinacci RM, Andraus W, De Paiva Haddad LB, Carneiro D’ Albuquerque LA, Herman P (2014) Simultaneous laparoscopic resection of primary colorectal cancer and associated liver metastases: a systematic review. Tech Coloproctol 18:129–135
Adam R, Chiche L, Aloia T et al (2006) Hepatic resection for noncolorectal nonendocrine liver metastases: analysis of 1452 patients and development of a prognostic model. Ann Surg 244:524
Osada S, Imai H, Sasaki Y, Tanaka Y, Tokuyama Y, Okumura N et al (2012) Strategy for synchronous and multiple liver metastasis. Hepatogastroenterology 59:198–203
Vladov N, Vasilevski I, Takorov I, Mutafchiyski V, Sergeev S, Odiseeva E et al (2012) Rational surgical aggression in multimodal treatment of liver colorectal metastases. Hepatogastroenterology 59:241–244
Quan D, Gallinger S, Nhan C, Auer RA, Biagi JJ, Fletcher GG et al (2013) The role of liver resection for colorectal cancer metastases in an era of multimodality treatment: a systematic review. Surgery 153(3):438
Spelt L, Andersson B, Nilsson J, Andersson R (2012) Prognostic models for outcome following liver resection for colorectal cancer metastases: a systematic review. Eur J Surg Oncol 38(1):16–24
Nomi T, Fuks D, Kawaguchi Y et al (2015) Laparoscopic major hepatectomy for colorectal liver metastases in elderly patients: a single-center, case-matched study. Surg Endosc 29:1368–1375
Nomi T, Fuks D, Govindasamy M et al (2015) Risk factors for complications after laparoscopic major hepatectomy. Br J Surg 102:254–260
Nomi T, Fuks D, Kawaguchi Y et al (2015) Learning curve for laparoscopic major hepatectomy. Br J Surg 102:796–804
Parisi A, Trastulli S, Ricci F, Regina R, Cirocchi R, Grassi V, Gemini A, Pironi D, D’Andrea V, Santoro A, Desiderio J (2016) Analysis of long-term results after liver surgery for metastases from colorectal and non-colorectal tumors: a retrospective cohort study. Int J Surg 30:25–30
Kassahun WT (2015) Controversies in defining prognostic relevant selection criteria that determine long-term effectiveness of liver resection for noncolorectal nonneuroendocrine liver metastasis. Int J Surg 24(Pt A):85–90
O’Rourke TR, Tekkis P, Yeung S, Fawcett J, Lynch S, Strong R, Wall D, John TG, Welsh F, Rees M (2008) Long-term results of liver resection for non-colorectal, non-neuroendocrine metastases. Ann Surg Oncol 15:207–218
Fitzgerald TL, Brinkley J, Banks S, Vohra N, Englert ZP, Zervos EE (2014) The benefits of liver resection for non-colorectal, nonneuroendocrine liver metastases: a systematic review. Langenbecks Arch Surg 399:989–1000
Uggeri F, Ronchi PA, Goffredo P et al (2015) Metastatic liver disease from noncolorectal, non-neuroendocrine, non-sarcoma cancers: a systematic review. World J Surg Oncol 13:191
Groeschl RT, Nachmany I, Steel JL et al (2012) Hepatectomy for noncolorectal non-neuroendocrine metastatic cancer: a multi-institutional analysis. J Am Coll Surg 214(5):769–777
Azoulay D, Castaing D, Krissat J, Smail A, Hargreaves GM, Lemoine A, Emile JF, Bismuth H (2000) Percutaneous portal vein embolization increases the feasibility and safety of major liver resection for hepatocellular carcinoma in injured liver. Ann Surg 232:665–672
Strasberg SM, Phillips C (2013) Use and dissemination of the brisbane 2000 nomenclature of liver anatomy and resections. Ann Surg 257:377–382
Tranchart H, Gaillard M, Chirica M, Ferretti S, Perlemuter G, Naveau S, Dagher I (2015) Multivariate analysis of risk factors for postoperative complications after laparoscopic liver resection. Surg Endosc 29:2538–2544
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D et al (2005) The ‘50–50 criteria’ on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242:824–828
Ishizawa T, Hasegawa K, Kokudo N et al (2009) Risk factors and management of ascites after liver resection to treat hepatocellular carcinoma. Arch Surg 144:46–51
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688
Rahbari NN, Garden OJ, Padbury R, Maddern G, Koch M, Hugh TJ et al (2011) Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford) 13:528–535
Frilling A, Modlin IM, Kidd M, Russell C, Breitenstein S, Salem R, Kwekkeboom D, Lau WY, Klersy C, Vilgrain V, Davidson B, Siegler M, Caplin M, Solcia E, Schilsky R, Working Group on Neuroendocrine Liver Metastases (2014) Recommendations for management of patients with neuroendocrine liver metastases. Lancet Oncol 15(1):e8–e21
Jagannath P, Chhabra D, Shrikhande S, Shah R (2012) Surgical treatment of liver metastases in neuroendocrine neoplasms. Int J Hepatol 2012:782672
Lee SY, Cheow PC, Teo JY, Ooi LL (2012) Surgical treatment of neuroendocrine liver metastases. Int J Hepatol 2012:146590
Neri F, Ercolani G, Di Gioia P, Del Gaudio M, Pinna AD (2015) Liver metastases from non-gastrointestinal non-neuroendocrine tumours: review of the literature. Updates Surg 67(3):223–233
Lehner F, Ramackers W, Bektas H, Becker T, Klempnauer J (2009) Liver resection for non-colorectal, non-neuroendocrine liver metastases e is hepatic resection justified as part of the oncosurgical treatment? Zentralbl Chi 135:430e6
Gurusamy KS, Ramamoorthy R, Sharma D, Davidson BR (2009) Liver resection versus other treatments for neuroendocrine tumors in patients with respectable liver metastases. Cochrane Database Syst Rev 15(2):CD007060
Maeda Y, Shinohara T, Katayama T, Futakawa N, Hamada T (2015) Hepatectomy for liver metastases in non-colorectal, non-neuroendocrine cancer patients. The survival benefit in primary unresectable cases. Int J Surg. 22:136–142
Slotta JE, Schuld J, Distler S, Richter S, Schilling MK, Kollmar O (2014) Hepatic resection of non-colorectal and non-neuroendocrine liver metastases—survival benefit for patients with non-gastrointestinal primary cancers—a case-controlled study. Int J Surg 12(2):163–168
Mayo SC, de Jong MC, Pulitano C et al (2010) Surgical management of hepatic neuroendocrine tumor metastasis: results from an international multi-institutional analysis. Ann Surg Oncol 17:3129–3136
Ercolani G, Grazi GL, Ravaioli M et al (2005) The role of liver resections for noncolorectal, nonneuroendocrine metastases: experience with 142 observed cases. Ann Surg Oncol 12:459–466
Page AJ, Weiss MJ, Pawlik TM (2014) Surgical management of noncolorectal cancer liver metastases. Cancer 120:3111–3121
Goumard C, Fuks D, Cauchy F, Belghiti J, Paugam-Burtz C, Castier Y, Soubrane O (2016) Pleural empyema following liver resection: a rare but serious complication. World J Surg 40(12):2999–3008
Lee KF, Wong J, Cheung SYS, Chong CCN, Hui JWY, Leung VYF, Yu SCH, Lai PBS (2018) Does intermittent pringle maneuver increase postoperative complications after hepatectomy for hepatocellular carcinoma? A randomized controlled trial. World J Surg 42(10):3302–3311
Kazaryan AM, Marangos IP, Rosok BI et al (2010) Laparoscopic resection of colorectal liver metastases: surgical and long-term oncologic outcome. Ann Surg 252:1005–1012
Ercolani G, Vetrone G, Grazi GL et al (2009) The role of liver surgery in the treatment of non-colorectal non-neuroendocrine metastases (NCRNNE). Analysis of 134 resected patients. Minerva Chir 64:551–558
Lendoire J, Moro M, Andriani O et al (2007) Liver resection for noncolorectal, non-neuroendocrine metastases: analysis of a multicenter study from Argentina. HPB (Oxford) 9:435–439
Pavel M, O’Toole D, Costa F et al (2016) ENETS consensus guidelines update for the management of distant metastatic disease of intestinal, pancreatic, bronchial neuroendocrine neoplasms (NEN) and NEN of unknown primary site. Neuroendocrinology 103:172–185
Saxena A, Chua TC, Perera M et al (2012) Surgical resection of hepatic metastases from neuroendocrine neoplasms: a systematic review. Surg Oncol 21:e131–e141
Sutcliffe R, Maguire D, Ramage J, Rela M, Heaton N (2004) Management of neuroendocrine liver metastases. Am J Surg 187:39–46
Musunuru S, Chen H, Rajpal S et al (2006) Metastatic neuroendocrine hepatic tumors: resection improves survival. Arch Surg 141:1000–1004
Sarmiento JM, Heywood G, Rubin J, Ilstrup DM, Nagorney DM, Que FG (2003) Surgical treatment of neuroendocrine metastases to the liver: a plea for resection to increase survival. J Am Coll Surg 197(1):29–37
Glazer ES, Tseng JF, Al-Refaie W et al (2010) Long-term survival after surgical management of neuroendocrine hepatic metastases. HPB (Oxford). 12(6):427–433
Cho CS, Labow DM, Tang L et al (2008) Histologic grade is correlated with outcome after resection of hepatic neuroendocrine neoplasms. Cancer 113(1):126–134
Schmelzle M, Eisenberger CF, Am Esch JS 2nd, Matthaei H, Krausch M, Knoefel WT (2010) Non-colorectal, non-neuroendocrine, and non-sarcoma metastases of the liver: resection as a promising tool in the palliative management. Langenbecks Arch Surg 395:227–234
Martel G, Hawel J, Rekman J, Croome KP, Bertens K, Balaa FK, Hernandez-Alejandro R (2015) Liver resection for non-colorectal, noncarcinoid, non-sarcoma metastases: a multicenter study. PLoS ONE 10:e0120569
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr Ioannis Triantafyllidis, Prof Brice Gayet, Dr Sofia Tsiakyroudi, Dr Nicolas Tabchouri, Prof Marc Beaussier, Dr Mostefa Bennamoun, Dr Anthony Sarran, Dr Marine Lefevre, Prof Christophe Louvet, and Prof David Fuks, all have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Triantafyllidis, I., Gayet, B., Tsiakyroudi, S. et al. Perioperative and long-term outcomes of laparoscopic liver resections for non-colorectal liver metastases. Surg Endosc 34, 3833–3844 (2020). https://doi.org/10.1007/s00464-019-07148-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07148-4