Abstract
Background
Postoperative venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), are the leading causes of morbidity and mortality after bariatric surgery. Although several studies have examined VTE, few have examined risk factors separately for DVT and PE after contemporary bariatric surgery, including laparoscopic sleeve gastrectomy (LSG). Our objective was to define risk factors for DVT and PE independently for both LSG and laparoscopic Roux-en-Y gastric bypass (LRYGB) patients using the largest validated bariatric surgery database.
Methods
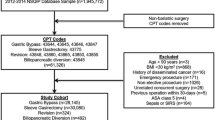
The metabolic and bariatric surgery accreditation and quality improvement program (MBSAQIP) database was queried to identify patients who underwent LSG or LRYGB between January 2015 and December 2017. Perioperative data were compared using bivariate analysis. Risk of DVT and PE after LSG or LRYGB was determined using multivariable logistic regression analysis.
Results
During the study period, 369,032 bariatric cases (72% LSG, 28% LRYGB) were performed. The incidence of DVT was similar between LSG and LRYGB (0.2% vs. 0.2%, p = 0.96), while the incidence of PE was decreased for LSG compared to LRYGB (0.1% vs. 0.2%, p < 0.001). Operative length was associated with increased risk of postoperative DVT (OR 1.1, CI 1.01–1.30, p = 0.04) and postoperative PE (OR 1.4, CI 1.16–1.64, p < 0.001) after surgery. The largest independent risk factors for DVT were history of DVT (OR 6.2, CI 4.44–8.45, p < 0.001) and transfusion (OR 4.2, CI 2.48–6.63, p < 0.001). The largest independent risk factors for PE were transfusion (OR 5.0, CI 2.69–8.36, p < 0.001) and history of DVT (OR 2.8, CI 1.67–4.58, p < 0.001). LSG was associated with a decreased risk of PE compared to LRYGB (OR 0.7 CI 0.55–0.91, p = 0.01).
Conclusions
Prolonged operative length is associated with a higher risk of DVT and PE after either LSG or LRYGB. Transfusion and history of DVT are the largest risk factors for developing DVT and PE. There is a decreased risk of PE after LSG compared to LRYGB.
Similar content being viewed by others
References
Aminian A, Andalib A, Khorgami Z et al (2017) Who should get extended thromboprophylaxis after bariatric surgery?: a risk assessment tool to guide indications for post-discharge pharmacoprophylaxis. Ann Surg 265(1):143–150
Masoomi H, Buchberg B, Reavis KM et al (2011) Factors predictive of venous thromboembolism in bariatric surgery. Am Surg 77(10):1403–1406
Escalante-Tattersfield T, Tucker O, Fajnwaks P, Szomstein S, Rosenthal RJ (2008) Incidence of deep vein thrombosis in morbidly obese patients undergoing laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 4(2):126–130
Stein PD, Matta F (2013) Pulmonary embolism and deep venous thrombosis following bariatric surgery. Obes Surg 23(5):663–668
Guerrier JB, Dietch ZC, Schirmer BD, Hallowell PT (2018) Laparoscopic sleeve gastrectomy is associated with lower 30-day morbidity versus laparoscopic gastric bypass: an analysis of the American college of surgeons NSQIP. Obes Surg 28(11):3567–3572
Dang JT, Switzer N, Delisle M et al (2018) Predicting venous thromboembolism following laparoscopic bariatric surgery: development of the BariClot tool using the MBSAQIP database. Surg Endosc 33(3):821
Chan MM, Hamza N, Ammori BJ (2013) Duration of surgery independently influences risk of venous thromboembolism after laparoscopic bariatric surgery. Surg Obes Relat Dis 9(1):88–93
Daigle CR, Brethauer SA, Tu C et al (2018) Which postoperative complications matter most after bariatric surgery? Prioritizing quality improvement efforts to improve national outcomes. Surg Obes Relat Dis 14(5):652–657
Bartlett MA, Mauck KF, Daniels PR (2015) Prevention of venous thromboembolism in patients undergoing bariatric surgery. Vasc Health Risk Manag 11:461–477
Jamal MH, Corcelles R, Shimizu H et al (2015) Thromboembolic events in bariatric surgery: a large multi-institutional referral center experience. Surg Endosc 29(2):376–380
Nguyen NT, Nguyen B, Smith B et al (2013) Proposal for a bariatric mortality risk classification system for patients undergoing bariatric surgery. Surg Obes Relat Dis 9(2):239–246
Moghadamyeghaneh Z, Hanna MH, Carmichael JC, Nguyen NT, Stamos MJ (2014) A nationwide analysis of postoperative deep vein thrombosis and pulmonary embolism in colon and rectal surgery. J Gastrointest Surg 18(12):2169–2177
Van Gent JM, Calvo RY, Zander AL et al (2017) Risk factors for deep vein thrombosis and pulmonary embolism after traumatic injury: a competing risks analysis. J Trauma Acute Care Surg 83(6):1154–1160
Finks JF, English WJ, Carlin AM et al (2012) Predicting risk for venous thromboembolism with bariatric surgery: results from the michigan bariatric surgery collaborative. Ann Surg 255(6):1100–1104
Wolberg AS, Aleman MM, Leiderman K, Machlus KR (2012) Procoagulant activity in hemostasis and thrombosis: virchow’s triad revisited. Anesthesia Analg 114(2):275–285
Xenos ES, Vargas HD, Davenport DL (2012) Association of blood transfusion and venous thromboembolism after colorectal cancer resection. Thromb Res 129(5):568–572
Nielsen AW, Helm MC, Kindel T et al (2018) Perioperative bleeding and blood transfusion are major risk factors for venous thromboembolism following bariatric surgery. Surg Endosc 32(5):2488–2495
Koh CY, Inaba CS, Sujatha-Bhaskar S et al (2017) Laparoscopic adjustable gastric band explantation and implantation at academic centers. J Am Coll Surg 225(4):532–537
Helm MC, Simon K, Higgins R, Kindel TL, Gould JC (2017) Perioperative complications increase the risk of venous thromboembolism following bariatric surgery. Am J Surg 214(6):1135–1140
Acknowledgements
We acknowledge the Center for Statistical Consulting at the University of California, Irvine for assistance in statistical analysis.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Ninh T. Nguyen has received honorarium as a speaker for Covidien, Gore, Novadaq, and Olympus. Dr. Brian R. Smith has received honorarium as an educational consultant for STRYKER Endoscopy. Dr. Sahil Gambhir, Dr. Colette Inaba, Dr. Reza F. Alizadeh, Dr. Shaun Daly, Dr. Jeffry Nahmias, and Dr. Marcelo Hinojosa have no conflicts of interest or financial ties to disclose. The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article. All authors have approved the final article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gambhir, S., Inaba, C.S., Alizadeh, R.F. et al. Venous thromboembolism risk for the contemporary bariatric surgeon. Surg Endosc 34, 3521–3526 (2020). https://doi.org/10.1007/s00464-019-07134-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07134-w