Abstract
Background
Transanal hybrid rectal and colon resection have been introduced in recent years at dedicated surgical centers. The anus is used as a natural orifice for large size access. The use of transanal hybrid colectomy techniques is still in its infancy with outcomes and unique complications being identified. The purpose of this work is the evaluation of outcomes for transanal hybrid colon resections (ta-CR), including intra operative and postoperative complications, results, and advantages.
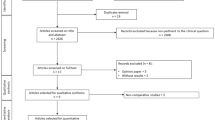
Methods
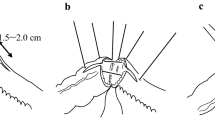
A prospectively maintained database was analyzed. Inclusion criteria were any patient who underwent ta-CR for rectal prolapse, slow transit, obstructive defaecation, and chronic sigmoid diverticulitis. Patients were excluded from ta-CR if BMI > 30, major previous abdominal surgery, or presence of a large inflammatory mass in diverticulitis. Transanal access was used for all operative steps requiring access of more than 5 mm, such as staplers, large graspers, and specimen retrieval. Data acquisition and analysis was performed for operative time, complications, and postoperative quality of life.
Results
From 2012 to 2017, 82 patients underwent ta-CR [33 males, 49 females, median age 58 (24–80)]. Transanal-subtotal colectomy and ta-CR for constipation was performed in 12 patients; ta-CR and rectopexy in 31, and ta-CR for diverticulitis was performed in 39 patients. Conversion to traditional approach was required in 3 cases (3.6%). Intraoperative complication included 1 rectal tear requiring intervention. Post-op complications included 3 leaks requiring laparoscopic and 1 open revision, the latter developed wound infection and an incisional hernia. Gastrointestinal Quality of Life Index (GIQLI) improved significantly from preoperative 89 to postoperative 119 (p < 0.001). No patients with ta-CR without open revision developed a hernia post-op with median 18 months follow-up.
Conclusions
ta-CR is a safe and effective NOTES Hybrid technique for colorectal procedures in selected patients with benign colon disorders. GIQLI shows improvement and this technique can have the potential in preventing wound and hernia complications.


Similar content being viewed by others
References
Rattner D, Hawes R, Schwaitzberg S, Kochman M, Swanstrom L (2011) The second SAGES/ASGE white paper on natural orifice translumenal endoscopic surgery: 5 years of progress. Surg Endosc 25:2441–2448
Fuchs KH, Meining A, von Renteln D, Fernandez-Esparrach G, Breithaupt W, Zornig C, Lacy A (2013) The EuroNOTES Status Paper—NOTES from the concept to clinical practice. Surg Endosc 27:1456–1467
Wolthuis AM, de Buck van Overstraeten A, D`Hoore A (2014) Laparoscopic natural orifice specimen extraction—colectomy: a systematic review. World J Gastroenterol 20(36):12981–12992
Zattoni D, Popeskou GS, Christoforidis D (2018) Left colon resection with transrectal specimen extraction: current status. Tech Coloproctol. https://doi.org/10.1007/s10151-018-1806-1
Buess G, Mentges B, Manncke K, Starlinger M (1992) Technique and results of transanal endoscopic microsurgery in early rectal cancer. Am J Surg 163:63–69
Allaix ME, Rebecchi F, Giaccone C, Mistrangelo M, Morino M (2011) Long-term functional results and quality of life after transanal endoscopic microsurgery. Br J Surg 98(11):1635–1643
Lirici MM, DiPaola M, Ponzano C, Hüscher GC (2003) Combining ultrasonic dissection and the Storz operation rectoscope. Surg Endosc 17(8):1292–1297
Sylla P, Willingham FF, Sohn DK, Brugge WR, Rattner DW (2008) NOTES rectosigmoid resection using transanal endoscopic microsurgery (TEM) with transgastric endoscopic assistance: a pilot study in swine. J Gastrointest Surg 12(10):1717–1723
Denk PM, Swanstrom LL, Whiteford MH (2008) Transanal endoscopic Microsurgical platform for natural orifice surgery. Gastrointest Endosc 68(5):954–959
Sylla P, Rattner DW, Delgado S, Lacy AM (2010) NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc 24(5):1205–1210
Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, Moran B, Hanna GB, Mortensen NJ, Tekkis PP (2017) taTME registry collaborative, transanal total mesorectal excision: international registry results of the first 720 Cases. Ann Surg 266(1):111–117
Deijen CL, Tsai A, Koedam TW, Veltcamp Helbach M, Sietses C, Lacy AM, Bonjer HJ, Tuynman JB (2016) Clinical outcomes and case volume effect of transanal total mesorectal excision for rectal cancer: a systematic review. Tech Coloproctol 20(12):811–824
McLemore EC, Harnsberger CR, Broderick RC, Leland H, Sylla P, Coker AM, Fuchs HF, Jacobsen GR, Sandler B, Attaluri V, Tsay AT, Wexner SD, Talamini MA, Horgan S (2016) Transanal total mesorectal excision (taTME) for rectal cancer: a training pathway. Surg Endosc 30(9):4130
Saad S, Hosogi H (2011) Laparoscopic left colectomy combined with natural orifice access: operative technique and initial results. Surg Endosc 25(8):2742–2747
Leroy J, Diana M, Wall J, Costantino F, D´Agostino J, Marescaux J (2011) Laparo-endoscopic single-site (LESS) with transanal natural orifice specimen extraction (NOSE) sigmoidectomy:a new step before pure colorectal natural orifices transluminal endoscopic surgery (NOZES). J Gastrointest Surg 15(8):1488–1492
Wolthuis AM, Meuleman C, Tomassetti C, D`Hooghe T, Fieuws S, Penninckx F, D´Hoore A (2011) Laparoscopic sigmoid resection with transrectal specimen extraction: a novel technique for the treatment of bowel endometriosis. Hum Reprod 26(6):1348–1355
Fuchs KH, Breithaupt W, Varga G, Schulz T, Reinisch A, Josipvic N (2013) Transanal Hybrid Colon resection – from laparoscopy to NOTES. Surg Endosc 27:746–752
Brockhaus AC, Politt D, Lindlohr C, Saad S (2016) Transanal extraction vs minilaparotomy lefr-sided colon resection. Chirurg 87(12):1054–1062
Arezzo A, Zornig C, Mofid H, Fuchs KH, Breithaupt W, Noguera J, Kaehler G, Magdeburg R, Perretta S, Dallemagne B, Marescaux J, Copaescu C, Graur F, Szasz A, Forgione A, Pugliese R, Buess G, Bhattacherjee HK, Navarra G, Godina M, Shishin K, Morino M (2013) The EURO-NOTES clinical registry for natural orifice transluminal endoscopic surgery: a 2-year activity report. Surg Endosc 27(9):3073–3084
Vlek SL, Lier MC, Koedam TW, Melgers I, Dekker JJ, Bonjier JH, Mijatovic V, Tuynman JB (2017) Transanal minimally invasive rectal resection for deep endometriosis; a promising technique. Colorectal Dis 19(6):576–581
Eypasch E, Williams JI, Wood-Dauphinee S, Ure BM, Schmulling C, Neugebauer E, Troidl H (1995) Gastrointestinal Quality of Life Index (GIQLI), development, validation and application of a new instrument. Br J Surg 82(2):216–222
Kim ER, Rhee PL (2012) How to interpret a functional or Motility Test—Colon transit study. J Neurogastroenterol Motil 18:94–99
Hussain A, Mahmood H, Singhal T, Balakrishnan S, Nicholls J, El-Hasani S (2009) Long-term study of port-site incisional hernia after laparoscopic procedures. JSLS 13(3):346–349
Holihan JL, Chen JS, Greenberg J, Hehir D, Johnston SM, Marcus D, Ryan H, Tsuda S, Liang MK (2016) Incidence of port-site hernias: a survey and literature review. Surg Laparosc Endosc Percutan Tech 26(6):425–430
Schey R, Cromwell K, Rao SS (2012) Medical and surgical management of pelvic floor disorders affecting defecation. Am J Gastroenterol 107(11):1624–1633
Matzel KE, Kamm MA, Stösser M (2004) Sacral spinal nerve stimulation for faecal incontinence: multicentre study. The Lancet 363:1270–1276
Kenefick NJ (2006) Sacral nerve neuromodulation for the treatment of lower bowel motility disorders. Ann R Coll Surg Engl 88:617–623
Ratto C, Ganio E, Naldini G, GINS (2015) Long-term results following sacral nerve stimulation for chronic constipation. Colorectal Dis 17:320–328
Thaha MA, Abukar AA, Thin NN, Ramsanahie A, Knowles C (2015) Sacral nerve stimulation for faecal incontinence and constipation. Cochrane Database Syst Rev 24:CD004464
Keller J, Bassotti G, Clarke J (2018) Advances in the diagnosis and classification of gastric and intestinal motility disorders. Nat Rev Gastroenterol Hepatol 15:291–308
Johnson E, Kjellevold K, Johannessen HO, Drolsum A (2012) Long-term outcome after resection rectopexy for internal rectal intussusception. ISRN Gastroenterol 2012:824671
Conston ECJ, van Iersel JJ, Verheiijen PM, Broeders IAMJ, Wolthuis AM, D´Hoore A (2015) Long-term outcome after laparoscopic ventral mesh rectopexy. Ann Surg 262:742–748
Tou S, Brown SR, Nelson RL (2015) Surgery for complete (full-thickness) rectal prolapse in adults. Cochrane Database Syst Rev 24(11):001758
Carvalho MEC, Hull T, Zutshi M, Gurland BH (2018) Resection rectopexy is still an acceptable operation for rectal prolapse. Am Surg 84(9):1470–1475
Anderweg CS, Berg R, Staal JB, ten Broek RP, van Goor H (2016) Patient-reported outcomes after conservative or surgical management of recurrent and chronic complaints of diverticulitis: systematic review and meta-analysis. Clin Gastroenterol Hepatol 14(2):183–190
Shaffer VO, Babtiste CD, Lio Y, Srinivasan JK, Galloway JR, Sullivan PS, Staley CA, Sweeney JF, Sharma J, Gillespie TW (2014) Improving quality of surgical care and outcomes: factors impacting surgical site infection after colorectal resection. Am Surg 80(8):759–763
Yamamoto M, Tanaka K, Asakuma M, Kondo K, Isii M, Hamamoto H, Okuda J, Uchiyama K (2015) Does transumbilical incision influence surgical site infection rates of the laparoscopic sigmoidectomy and anterior resection? Am Surg 81(12):1232–1236
Conolly TM, Foppa C, Kazi E, Denoya PI, Bergamaschi R (2016) Impact of a surgical site infection reduction strategy after colorectal resection. Colorectal Dis 18(9):910–918
Tonouchi H, Ohmori Y, Kobayashi M, Kusunoki M (2004) Trocar site hernia. Arch Surg 139(11):1248–1256
Lee L, Mappin-Kasirer B, Sender Liberman A, Stein B, Charlebois P, Vassiliu M, Fried GM, Feldmann LS (2012) High incidence of symptomatic incisional hernia after midline extraction in laparoscopic colon resection. Surg Endosc 26(11):3180–3185
Campagnacci R, Baldoni A, Ghiselli R, Cappelletti-Trombettoni MM, Guerrieri M (2015) Prevention of hernia incision in laparoscopic left colon resection. Miverva Chir 70(3):155–160
Blumetti J, Abcarian H (2015) Management of low colorectal anastomotic leak: preserving the anastomosis. World J Gastrointest Surg 7(12):378–383
Diana M, Wall J, Costantino F, Leroy DJ, Marescaux J (2011) Transanal extraction of the specimen during laparoscopic colectomy. Colorectal Dis. https://doi.org/10.1111/j.1463-1318.2011.02774.x
Franklin ME Jr, Liang S, Russek K (2013) Natural orifice specimen extraction in laparoscopic colorectal surgery: transanal and transvaginal approaches. Tech Coloproctol 17(Suppl 1):S63–S67
Vahdad MR, Cernaianu G, Semaan A, Klein T, Faran S, Zemon H, Boemers T, Foroutan HR (2016) An experimental study in six fresh human cadavers using a novel approach to avoid abdominal wall incisions in total colectomy: totally transanal laparoendoscopic single-site pull-through colectomy with j-pouch creation. Surg Endosc 30(7):3107–3113
Karagul S, Kayaalp C, Sumer F, Ertgru I, Kirmizi S, Tardu A, Yagci MA (2017) Success rate of natural orifice specimen extraction after laparoscopic resections. Tech Coloproctol 21(4):295–300
Funding
This project has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Karl-Hermann Fuchs declares that he is a consultant to Olympus Europe Holding SE&Co.KG, Hamburg, Germany and Consultant to MedeServ GbR Winterburg, Germany. These two companies were involved in the development and distribution of the TEA device (Transanal Endoscopic Applicator). Thomas Schulz, Ryan Broderick, Wolfram Breithaupt, Benjamin Babic, Gabor Varga, Santiago Horgan declares that they have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fuchs, KH., Schulz, T., Broderick, R. et al. Transanal hybrid colon resection: techniques and outcomes for benign colorectal diseases. Surg Endosc 34, 3487–3495 (2020). https://doi.org/10.1007/s00464-019-07126-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07126-w