Abstract
Background
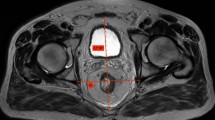
Total mesorectal excision (TME) is challenging to perform in a deep, narrow pelvis. While previous studies used pelvimetry to assess bony pelvic structures, there is no consensus on exact definition of deep, narrow pelvis. We hypothesized that the shape of pelvic floor muscle may impact the performance of transabdominal pelvic dissection. We aimed to evaluate which parameters of the shape of pelvic floor muscle impact the difficulty of TME and present a predictive reference value for TME difficulty.
Methods
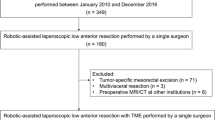
From January 2015 to December 2015, 85 consecutive patients who had undergone curative resection for middle to lower rectal cancer were retrospectively studied. Pelvimetry was performed using preoperative T2-weighted magnetic resonance imaging. Predictive factor analysis for surgical duration was studied using linear regression. Mann–Whitney U test, comparing surgical duration between two groups classified by predictive factor, was used for the analysis of reference value.
Results
Multivariate analysis revealed that body mass index, protective stoma, number of surgeon, and incline angle of pelvic floor muscle (β) were independent predictors of surgical duration. Test statistics of Mann–Whitney U for the difference in surgical duration between groups above and below a β of 54° were maximized.
Conclusions
The incline angle of pelvic floor muscle is an independent predictor of surgical duration. In patients with steeper incline of PFM, transabdominal TME is expected to be difficult. This index is novel, but needs to be further validated.




Similar content being viewed by others
References
Zhou X, Su M, Hu K, Su Y, Ye Y, Huang C, Yu Z, Li X, Zhou H, Ni Y, Jiang Y (2015) Applications of computed tomography pelvimetry and clinical-pathological parameters in sphincter preservation of mid-low rectal cancer. Int J Clin Exp Med 15:2174–2181
Kim JY, Kim YW, Kim NK, Hur H, Lee K, Min BS, Cho HJ (2011) Pelvic anatomy as a factor in laparoscopic rectal surgery: a prospective study. Surg Laparosc Endosc Percutan Tech 21:334–339
Zhou XC, Su M, Hu KQ, Su YF, Ye YH, Huang CQ, Yu ZL, Li XY, Zhou H, Ni YZ, Jiang YI, Lou Z (2016) CT pelvimetry and clinicopathological parameters in evaluation of the technical difficulties in performing open rectal surgery for mid-low rectal cancer. Oncol Lett 11:31–38
Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Miyata S, Yamaguchi T (2009) Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery 146:483–489
Baik SH, Kim NK, Lee KY, Sohn SK, Cho CH, Kim MJ, Kim H, Shinn RK (2008) Factors influencing pathologic results after total mesorectal excision for rectal cancer: analysis of consecutive 100 cases. Ann Surg Oncol 15:721–728
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH (2002) Cooperative Clinical Investigators of the Dutch Colorectal Cancer Group. Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20:1729–1734
Targarona EM, Balague C, Pernas JC, Martinez C, Berindoague R, Gich I, Trias M (2008) Can we predict immediate outcome after laparoscopic rectal surgery? Multivariate analysis of clinical, anatomic, and pathologic features after 3-dimensional reconstruction of the pelvic anatomy. Ann Surg 247:642–649
Guo M, Li D (2007) Pelvic floor images: anatomy of the levator ani muscle. Dis Colon Rectum 50:1647–1655
Yamaoka Y, Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y, Furutani A, Manabe S, Torii K, Koido K, Mori K (2019) Mesorectal fat area as a useful predictor of the difficulty of robotic-assisted laparoscopic total mesorectal excision for rectal cancer. Surg Endosc 33(2):557–566
Penna M, Cunningham C, Hompes R (2017) Transanal total mesorectal excision: why, when, and how. Clin Colon Rectal Surg 30:339–345
Simillis C, Hompes R, Penna M, Rasheed S, Tekkis PP (2016) A systematic review of transanal total mesorectal excision: is this the future of rectal cancer surgery? Colorectal Dis 18:19–36
Motson RW, Whiteford MH, Hompes R, Albert M, Miles WF (2016) Current status of trans-anal total mesorectal excision (TaTME) following the Second International consensus conference. Colorectal Dis 18:13–18
Acknowledgements
The authors would like to thank Joon Seok Lim, the radiologist for methodological advice in pelvimetry, for helping with this study. Financial support for English proofreading was provided by Yonsei University College of Medicine.
Funding
No financial support.
Author information
Authors and Affiliations
Contributions
Conception and design: JML and NKK; Collection and assembly of data: JML; Data analysis and interpretation: JML, YDH, MSC, HH, BSM, and KYL.; Manuscript writing: All authors; Final approval of manuscript: All authors.
Corresponding author
Ethics declarations
Disclosures
Jong Min Lee, Yoon Dae Han, Min Soo Cho, Hyuk Hur, Byung Soh Min, Kang Young Lee, and Nam Kyu Kim have no conflicts of interest or financial ties to disclose.
Ethics approval
The study protocol was approved by the Institutional Review Board at Human Research Protection Center of Severance Hospital in Seoul, South Korea (4-2018-0447). Informed consent was waived due to the retrospective analysis of this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimers The content of this study is under the responsibility of the authors, and the opinions contained herein may not reflect the official views of Yonsei University College of Medicine.
Rights and permissions
About this article
Cite this article
Lee, J.M., Han, Y.D., Cho, M.S. et al. Prediction of transabdominal total mesorectal excision difficulty according to the angle of pelvic floor muscle. Surg Endosc 34, 3043–3050 (2020). https://doi.org/10.1007/s00464-019-07102-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07102-4