Abstract
Introduction
Per-Oral Endoscopic Myotomy (POEM) is a less invasive alternative to laparoscopic Heller myotomy for patients with achalasia. While a partial fundoplication is often performed concurrently with laparoscopic myotomy, an endoscopic approach does not offer this and leaves patients prone to post-operative reflux. The objectives of this study were to (1) identify patients with post-POEM reflux using BRAVO pH and endoscopic evaluations, and (2) investigate risk factors associated with post-POEM reflux and esophagitis to optimize patient selection for POEM and identify those who will benefit from a proactive approach to post-operative reflux management.
Methods
A retrospective review of a prospectively collected database of patients who underwent POEM between January 2011 and July 2017 at a single institution was performed. Demographics along with pre-POEM and post-POEM variables were obtained. Univariate and multivariate analyses were performed, using p values ≤ 0.05 for statistical significance.
Results
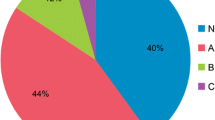
Forty-six patients were included, with a mean follow-up of 358 days. Mean age was 58 (19.2); 61% were female. Thirty-six patients underwent 48-h BRAVO pH testing after POEM, which revealed abnormal esophageal acid exposure in 15 patients (41.7%). There was a correlation between positive BRAVO results and presence of preoperative esophagitis (p = 0.02). Only 13% of patients had symptom-related reflux episodes based on the Symptom Associated Probability of the BRAVO study. Post-operative endoscopy revealed 6 patients with esophagitis, compared to 4 patients who had esophagitis on preoperative endoscopy. Only higher preoperative Eckardt score was significantly associated with endoscopic evidence of esophagitis post-POEM.
Conclusions
Reflux is common after POEM. A majority of patients with a positive BRAVO study are asymptomatic, which is concerning. Objective follow-up is of paramount importance with upper endoscopy and ambulatory pH monitoring being the gold standard. Elevated preoperative Eckardt score and esophagitis are associated with post-POEM reflux. This population warrants close surveillance.
Similar content being viewed by others
References
Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108(8):1238–1249
Kahrilas PJ, Bredenoord AJ, Fox M et al (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27(2):160–174
Cheatham JG, Wong RK (2011) Current approach to the treatment of achalasia. Curr Gastroenterol Rep 13(3):219–225
Moonen A, Annese V, Belmans A et al (2016) Long-term results of the European achalasia trial: a multicenter randomized controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 65(5):732–739
Campos GM, Vittinghoff E, Rabl C et al (2009) Endosocpic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 249(1):45–57
Inoue H, Minami H, Kobayaski Y et al (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42(4):265–271
Schneider AM, Louis BE, Warren HF, Farivar AS, Schembre DB, Aye RW (2016) A matched comparison of per oral endoscopic myotomy to laparoscopic heller myotomy in the treatment of achalasia. J Gastrointest Surg 20(11):1789–1796
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259(6):1098–1103
Richter JR (2013) Achalasia and lower esophageal sphincter anatomy and physiology: implications for per oral esophageal myotomy technique. Tech Gastrointest Endosc 15(3):122–126
Chander B, Hanley-Williams N, Deng Y, Sheth A (2012) 24 versus 48-hour BRAVO pH monitoring. J Clin Gastroenterol 46(3):197–200
Tseng D, Rizvi AZ, Fennerty MB et al (2005) Forty-eight-hour pH monitoring increases sensitivity in detecting abnormal esophageal acid exposure. J Gastrointest Surg 9(8):1043–1051
Jones EL, Meara MP, Schwartz JS, Hazey JW, Perry KA (2016) Gastroesophageal reflux symptoms do not correlate with objective pH testing after peroral endoscopic myotomy. Surg Endosc 30(3):947–952
Streets CG, DeMeester TRJ (2003) Ambulatory 24-hour esophageal pH monitoring: why, when and what to do. J Clin Gastroenterol 37(1):14–22
Li QL, Chen WF, Zhou PH et al (2013) Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg 217(3):442–451
Crookes PF, Corkill S, DeMeester TR (1997) Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Des Sci 42(7):1354–1361
Caciano SL, Inman CL, Gockel-Blessing EE, Weiss EP (2015) Effects of dietary acid load on exercise metabolism and anaerobic exercise performance. J Sports Sci Med 14(2):364–371
Park Y, Subar AF, Hollenbeck Am Schatzkin A (2011) Dietary fiber intake and mortality in the NIH-AARP diet and health study. Arch Intern Med 171(12):1061–1068
Tilg H, Moschen AR (2015) Food, immunity, and the microbiome. Gastroenterology 148(6):1107–1119
Angel KF, Marks JM (2017) The future of achalasia therapy: expanding the minimally invasive armamentarium and risk of secondary gastroesophageal reflux. J Thorac Dis 9(10):3659–3662
Familiari P, Greco S, Gigante G et al (2016) Gastroesophageal reflux disease after peroral endoscopic myotomy: analysis of clinical, procedural and functional factors, associated with gastroesophageal reflux disease and esophagitis. Dig Endosc 28(1):33–41
Sharata AM, Dunst CM, Pescarus R et al (2015) Peroral endoscopic myotomy (POEM) for esophageal primary motility disorders: analysis of 100 consecutive patients. J Gastrointest Surg 19(1):161–170
Gerson LB, Shetler K, Triadafilopoulos G (2002) Prevalence of Barrett’s esophagus in asymptomatic individuals. Gastroenterology 123(2):461–467
Zerbib F (2015) The prevalence of oesophagitis in “silent” gastro-oesophageal reflux disease: higher than expected? Dig Liver Dis 47(1):12–13
Kumta NA, Kedia P, Sethi A, Kahaleh M (2015) Transoral incisionless fundoplication for treatment of refractory GERD after peroral endoscopic myotomy. Gastointest Endosc 81(1):224–225
Tyberg A, Choi A, Gaidhane M, Kahaleh M (2018) Transoral incisionless fundoplication for reflux after peroral endoscopic myotomy: a crucial addition to our arsenal. Endosc Int Open 6(5):C2
Chavez YH, Ngamruengphong S, Bukhari M, Chen Y, Aguila G, Khashab MA (2017) Transoral incisionless endoscopic fundoplication guided by impedance planimetry to treat severe GERD symptoms after per-oral endoscopic myotomy. Gastrointest Endosc 85(1):254–255
Shiwaku H, Inoue H, Sasaki T et al (2016) A prospective analysis of GERD after POEM on anterior myotomy. Surg Endosc 30(6):2496–2504
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Marks has provided consultant services for Boston Scientific and Olympus. Drs. Arevalo, Sippey, Martin-del-Campo, and Ali have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.