Abstract
Introduction
Although bariatric center procedural volume has been associated with early perioperative safety, data on the effect of such volume and long-term outcomes after sleeve gastrectomy (SG) are limited. This study aims to examine the relationship between annual bariatric center SG volume and the incidence of revisions or conversions (RC) after SG.
Methods
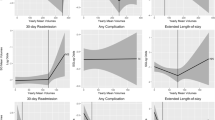
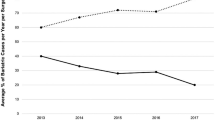
The New York Statewide Planning and Research Cooperative System database was used to identify all patients who underwent SG between 2006 and 2012. Subsequent RC events were captured up to 2016. Bariatric centers having annual SG volume less than 45, between 45 and 65, and greater than 65 were defined as low (LV), medium (MV), and high volume (HV), respectively. Multivariable Cox proportional hazard regression analysis was performed to compare the risk of having RC among centers with different yearly sleeve volumes.
Results
We identified 8389 patients who underwent SG. The overall estimated cumulative incidence of RC was 0.5% (95% CI 0.3–0.6%) at 1 year, 6.2% (95% CI 5.4–7.0%) at 5 years, and 15.3% (95% CI 12.6–18.0%) at 8 years after SG. The estimated cumulative incidence of RC for LV, MV, and HV at 8 years after SG was 16.7% (95% CI 11.1–22.3%), 15.5% (95% CI 11.2–19.8%), and 13.7% (95% CI 9.4–17.9%), respectively. HV centers have lower risk of RC compared to LV (hazard ratio 0.65; 95% CI 0.48–0.88) and MV (hazard ratio 0.75; 95% CI 0.57–0.98). LV and MV centers have comparable risk of RC (hazard ratio 1.15; 95% CI 0.87–1.51). Patients having the initial SG performed in LV were the least likely to have RC in the same institution (46.1% of LV, 13.2% of MV and 22.3% of HV; p < 0.0001).
Conclusion
Patients undergoing SG at LV centers experience the highest risk of subsequent RC. This effect persists after adjusting for patient-level factors. These data underline the relationship between volume threshold and long-term effect.

Similar content being viewed by others
References
Spaniolas K, Kasten KR, Brinkley J, Sippey ME, Mozer A, Chapman WH, Pories WJ (2015) The changing bariatric surgery landscape in the USA. Obes Surg 25(8):1544–1546
Casillas RA, Um SS, Zelada Getty JL, Sachs S, Kim BB (2016) Revision of primary sleeve gastrectomy to Roux-en-Y gastric bypass: indications and outcomes from a high-volume center. Surg Obes Relat Dis 12(10):1817–1825
Shimizu H, Annaberdyev S, Motamarry I, Kroh M, Schauer PR, Brethauer SA (2013) Revisional bariatric surgery for unsuccessful weight loss and complications. Obes Surg 23(11):1766–1773
Ibrahim AM, Thumma JR, Dimick JB (2017) Reoperation and medicare expenditures after laparoscopic gastric band surgery. JAMA Surg 152(9):835–842
Markar SR, Penna M, Karthikesalingam A, Hashemi M (2012) The impact of hospital and surgeon volume on clinical outcome following bariatric surgery. Obes Surg 22(7):1126–1134
Nguyen NT, Paya M, Stevens M, Mavandadi S, Zainabadi K, Wilson SE (2004) The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Ann Surg 240(4):586–593
Birkmeyer NJO, Dimick JB, Share D, Hawasli A, English WJ, Genaw J, Finks JF, Carlin AM, Birkmeyer JD (2010) Hospital complication rates with bariatric surgery in Michigan. JAMA 304(4):435–442
Celio AC, Kasten KR, Brinkley J, Chung AY, Burruss MB, Pories WJ, Spaniolas K (2016) Effect of surgeon volume on sleeve gastrectomy outcomes. Obes Surg 26(11):2700–2704
Celio AC, Kasten KR, Burruss MB, Pories WJ, Spaniolas K (2017) Surgeon case volume and readmissions after laparoscopic Roux-en-Y gastric bypass: more is less. Surg Endosc 31(3):1402–1406
Altieri MS, Yang J, Nie L, Blackstone R, Spaniolas K, Pryor A (2018) Rate of revisions or conversion after bariatric surgery over 10 years. Surg Obes Relat Dis 14(4):500–508
Andresen K, Friis-Andersen H, Rosenberg J (2016) Laparoscopic repair of primary inguinal hernia performed in public hospitals or low-volume centers have increased risk of reoperation for recurrence. Surg Innov 23(2):142–147
Harrison EM, O’Neill S, Meurs TS, Wong PL, Duxbury M, Paterson-Brown S, Wigmore SJ, Garden OJ (2012) Hospital volume and patient outcomes after cholecystectomy in Scotland: retrospective, national population based study. BMJ 344:e3330
Guller U, Warschkow R, Ackermann CJ, Schmied B, Cerny T, Ess S (2017) Lower hospital volume is associated with higher mortality after esophageal, gastric, pancreatic and rectal cancer resection. Swiss Med Wkly 147:w14473
Birkmeyer JD, Siewers AE, Finlayson EVA, Stukel TA, Lucas FL, Batista I, Welch HG, Wennberg DE (2002) Hospital Volume and surgical mortality in the United States. N Engl J Med 346(15):1128–1137
Finks JF, Osborne NH, Birkmeyer JD (2011) Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med 364(22):2128–2137
Killeen SD, Andrews EJ, Redmond HP, Fulton GJ (2007) Provider volume and outcomes for abdominal aortic aneurysm repair, carotid endarterectomy, and lower extremity revascularization procedures. J Vasc Surg 45(3):615–626
Eckstein HH, Bruckner T, Heider P, Wolf O, Hanke M, Niedermeier HP, Noppeney T, Umscheid T, Wenk H (2007) The relationship between volume and outcome following elective open repair of abdominal aortic aneurysms (AAA) in 131 German hospitals. Eur J Vasc Endovasc Surg 34(3):260–266
Katz JN, Barrett JA, Mahomed NN, Baron JA, Wright RJ, Losina E (2004) Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am 86(9):1909–1916
Katz JN, Mahomed NN, Baron JA, Barrett JA, Fossel AH, Creel AH, Wright J, Wright EA, Losina E (2007) Association of hospital and surgeon procedure volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum 56(2):568–574
Vree FEM, Cohen SL, Chavan N, Einarsson JI (2014) The impact of surgeon volume on perioperative outcomes in hysterectomy. JSLS 18(2):174–181
Unger CA, Lachiewicz MP, Ridgeway B (2016) Risk factors for robotic gynecologic procedures requiring conversion to other surgical procedures. Int J Gynaecol Obstet 135(3):299–303
Nimptsch U, Mansky T (2017) Hospital volume and mortality for 25 types of inpatient treatment in German hospitals: observational study using complete national data from 2009 to 2014. BMJ Open 7(9):e016184
Hannan EL, Kilburn H Jr, Bernard H, O’Donnell JF, Lukacik G, Shields EP (1991) Coronary artery bypass surgery: the relationship between inhospital mortality rate and surgical volume after controlling for clinical risk factors. Med Care 29(11):1094–1107
Zevin B, Aggarwal R, Grantcharov TP (2012) Volume-outcome association in bariatric surgery: a systematic review. Ann Surg 256(1):60–71
Hollenbeak CS, Rogers AM, Barrus B, Wadiwala I, Cooney RN (2008) Surgical volume impacts bariatric surgery mortality: a case for centers of excellence. Surgery 144(5):736–743
Luft HS, Hunt SS, Maerki SC (1987) The volume-outcome relationship: practice-makes-perfect or selective-referral patterns? Health Serv Res 22(2):157–182
Ibrahim AM, Ghaferi AA, Thumma JR, Dimick JB (2017) Variation in outcomes at bariatric surgery centers of excellence. JAMA Surg 152(7):629–636
Weller WE, Rosati C, Hannan EL (2007) Relationships between surgeon and hospital volume and readmission after bariatric operation. J Am Coll Surg 204(3):383–391
Acknowledgements
We acknowledge the biostatistical consultation and support from the biostatistical consultation and support from the Biostatistical Consulting Core at the School of Medicine, Stony Brook University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
No industry or other external funding was used for this research. Dr. Spaniolas receives research grant from Merck and is on the Advisory Board for Mallickrodt. Dr. Pryor receives honoraria for speaking for Ethicon, Medtronic, Stryker, and Gore and is a consultant for Merck, Obalon, and Baronova. Ms. Tsui, Dr. Yang, Mr. Nie, Dr. Altieri, and Dr. Talamini have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsui, S.T., Yang, J., Nie, L. et al. Association of revisions or conversions after sleeve gastrectomy with annual bariatric center procedural volume in the state of New York. Surg Endosc 34, 3110–3117 (2020). https://doi.org/10.1007/s00464-019-07068-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07068-3