Abstract
Background
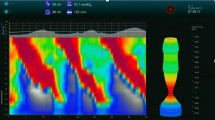
The functional luminal imaging probe (FLIP) can evaluate esophagogastric junction (EGJ) distensibility and esophageal peristalsis in real time. FLIP measurements performed during diagnostic endoscopy can accurately discriminate between healthy controls and patients with achalasia based on EGJ-distensibility and distinct motility patterns termed repetitive antegrade contractions (RACs) and repetitive retrograde contractions (RRCs). We sought to evaluate real-time motility changes in patients undergoing surgical myotomy for achalasia.
Methods
FLIP measurements using a stepwise volumetric distention protocol were performed at three time points during assessment and performance of laparoscopic Heller myotomy and POEM: (1) During preoperative outpatient endoscopy, (2) Intraoperatively following induction of anesthesia, and (3) Intraoperatively after myotomy completion. EGJ-distensibility, contractility, RACs, and RRCs were measured.
Results
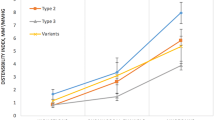
FLIP measurements were performed in 32 patients. The EGJ-distensibility index was similar between the preoperative and initial operative measurements (1.1 vs 1.4 mm2/mmHg, p = NS). There was a significant increase in distensibility following surgical myotomy (1.4 to 4.7 mm2/mmHg, p < 0.01). Intraoperative contractile patterns varied between achalasia subtypes. Contractility was seen in < 20% of assessments in patients with types I and II achalasia. Type III patients demonstrated contractility in 100% of assessments, with 70% exhibiting RRCs and 60% RACs. There was a reduction in the frequency of RRC presence (70% to 20%), and contractile vigor (80% to 0% of patients with lumen occluding contractions) in type III patients following surgical myotomy.
Conclusions
This first report of real-time intraoperative measurement of esophageal motility using FLIP demonstrates the feasibility of such assessments during surgical myotomy for achalasia. Patients with type I and II achalasia exhibited rare intraoperative contractility, while the presence of motility was the norm in those with type III. Patients with type III achalasia demonstrated an immediate reduction in repetitive contraction motility patterns and contractile vigor following myotomy.





Similar content being viewed by others
References
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet 383:83–93
Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE (2012) Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology 143:328–335
Teitelbaum EN, Boris L, Arafat FO, Nicodeme F, Lin Z, Kahrilas PJ, Pandolfino JE, Soper NJ, Hungness ES (2013) Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc 27:4547–4555
Ngamruengphong S, von Rahden BH, Filser J, Tyberg A, Desai A, Sharaiha RZ, Lambroza A, Kumbhari V, El Zein M, Abdelgelil A, Besharati S, Clarke JO, Stein EM, Kalloo AN, Kahaleh M, Khashab MA (2016) Intraoperative measurement of esophagogastric junction cross-sectional area by impedance planimetry correlates with clinical outcomes of peroral endoscopic myotomy for achalasia: a multicenter study. Surg Endosc 30:2886–2894
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Hirano I, Boris L, Nicodème F, Lin Z, Hungness ES (2015) Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc 29:522–528
Carlson DA, Lin Z, Rogers MC, Lin CY, Kahrilas PJ, Pandolfino JE (2015) Utilizing functional lumen imaging probe topography to evaluate esophageal contractility during volumetric distention: a pilot study. Neurogastroenterol Motil 27:981–989
Carlson DA, Kahrilas PJ, Lin Z, Hirano I, Gonsalves N, Listernick Z, Ritter K, Tye M, Ponds FA, Wong I, Pandolfino JE (2016) Evaluation of esophageal motility utilizing the functional lumen imaging probe. Am J Gastroenterol 111:1726–1735
Carlson DA, Lin Z, Kahrilas PJ, Sternbach J, Donnan EN, Friesen L, Listernick Z, Mogni B, Pandolfino JE (2015) The functional lumen imaging probe detects esophageal contractility not observed with manometry in patients with achalasia. Gastroenterology 149:1742–1751
Eckardt VF (2001) Clinical presentation and complications of achalasia. Gastrointest Endosc Clin N Am 11:281–292
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, Pandolfino JE (2015) The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Campagna RAJ, Hungness ES (2018) Treatment of idiopathic achalasia with per-oral esophageal myotomy. Tech Gastrointest Endosc 20:114–119
Vaziri K, Soper NJ (2008) Laparoscopic Heller myotomy: technical aspects and operative pitfalls. J Gastrointest Surg 12:1586–1591
Hirano I, Pandolfino JE, Boeckxstaens GE (2017) Functional lumen imaging probe for the management of esophageal disorders: expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol 15:325–334
van Herwaarden MA, Samsom M, Smout AJ (2001) Prolonged manometric recordings of oesophagus and lower oesophageal sphincter in achalasia patients. Gut 49:813–821
Bardan E, Xie P, Aslam M, Kern M, Shaker R (2000) Disruption of primary and secondary esophageal peristalsis by afferent stimulation. Am J Physiol Gastrointest Liver Physiol 279:G255–G261
Pandolfino JE, Shi G, Zhang Q, Kahrilas PJ (2005) Absence of a deglutitive inhibition equivalent with secondary peristalsis. Am J Physiol Gastrointest Liver Physiol 288:G671–G676
Sifrim D, Janssens J (1996) Secondary peristaltic contractions, like primary peristalsis, are preceded by inhibition in the human esophageal body. Digestion 57:73–78
Takeda T, Nabae T, Kassab G, Liu J, Mittal RK (2004) Oesophageal wall stretch: the stimulus for distension induced oesophageal sensation. Neurogastroenterol Motil 16:721–728
Rao SS, Hayek B, Summers RW (1995) Impedance planimetry: an integrated approach for assessing sensory, active, and passive biomechanical properties of the human esophagus. Am J Gastroenterol 90:431–438
Miyawaki I, Nakamura K, Terasako K, Toda H, Kakuyama M, Mori K (1995) Modification of endothelium-dependent relaxation by propofol, ketamine, and midazolam. Anesth Analg 81:474–479
Deutschman CS, Harris AP, Fleisher LA (1994) Changes in heart rate variability under propofol anesthesia: a possible explanation for propofol-induced bradycardia. Anesth Analg 79:373–377
Win NN, Fukayama H, Kohase H, Umino M (2005) The different effects of intravenous propofol and midazolam sedation on hemodynamic and heart rate variability. Anesth Analg 101:97–102
Aadam AA, Abe S (2018) Endoscopic submucosal dissection for superficial esophageal cancer. Dis Esophagus. https://doi.org/10.1016/S1542-3565(05)00291-0
Kraichely RE, Arora AS, Murray JA (2010) Opiate-induced oesophageal dysmotility. Aliment Pharmacol Ther 31:601–606
Ravi K, Murray JA, Geno DM, Katzka DA (2016) Achalasia and chronic opiate use: innocent bystanders or associated conditions? Dis Esophagus 29:15–21
Chen CL, Liu TT, Yi CH (2011) Control of esophageal distension-induced secondary peristalsis by the GABA(B) agonist baclofen in humans. Neurogastroenterol Motil 23:612-e250
Chen CL, Liu TT, Yi CH (2010) Effects of lidocaine on esophageal secondary peristalsis in humans. Neurogastroenterol Motil 22:606–610
Pitt KA, Mayhew PD, Barter L, Pollard R, Kass PH, Marks SL (2017) Consistency and effect of body position change on measurement of upper and lower esophageal sphincter geometry using impedance planimetry in a canine model. Dis Esophagus 30:1–7
Teitelbaum EN, Soper NJ, Pandolfino JE, Kahrilas PJ, Boris L, Nicodeme F, Lin Z, Hungness ES (2014) An extended proximal esophageal myotomy is necessary to normalize EGJ distensibility during Heller myotomy for achalasia, but not POEM. Surg Endosc 28:2840–2847
Nathanson LK, Brunott N, Cavallucci D (2012) Adult esophagogastric junction distensibility during general anesthesia assessed with an endoscopic functional luminal imaging probe (EndoFLIP(R)). Surg Endosc 26:1051–1055
Funding
This work was supported by R01 DK079902 (JEP) and P01 DK117824 (JEP) from the Public Health service. Ryan A. J. Campagna, MD is supported by T32DK101363 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Carlson: Medtronic, Inc.—speaking, consulting, shared intellectual property rights and ownership surrounding functional luminal imaging probe panometry systems, methods, and apparatus. Dr. Hungness: Cook Medical—consulting; Boston Scientific—consulting. Dr. Pandolfino: Medtronic, Inc.—consulting, grant funding, speaking, consulting, shared intellectual property rights and ownership surrounding functional luminal imaging probe panometry systems, methods, and apparatus; Sandhill Scientific—consulting, speaking; Crospon—stock options; Takeda—speaking; AstraZeneca—speaking. Dr. Soper: Miret Surgical, Inc.—scientific advisory board, stock options; FlexDex, Inc.—scientific advisory board, stock options; MeshSuture, Inc.—scientific advisory board, stock options. Dr. Teitelbaum: Cook Medical—consulting; Boston Scientific—consulting. Drs. Campagna and Holmstrom: None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Campagna, R.A.J., Carlson, D.A., Hungness, E.S. et al. Intraoperative assessment of esophageal motility using FLIP during myotomy for achalasia. Surg Endosc 34, 2593–2600 (2020). https://doi.org/10.1007/s00464-019-07028-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07028-x