Abstract
Background
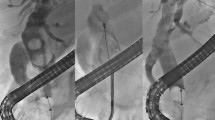
Standard endoscopic treatment might fail to treat biliary stone disease. Here, we investigated the efficacy and safety of recently introduced digital single-operator video cholangioscopy (SOVC) for the treatment of difficult biliary stones.
Methods
Digital SOVC procedures, performed in two tertiary referral centers between 2015 and 2018, were retrospectively analyzed. Only patients with a previous failure of endoscopic standard treatment and a SOVC-based biliary stone treatment using electrohydraulic lithotripsy (EHL) or laser lithotripsy (LL) were included. The primary endpoint was to evaluate the stone removal rate per procedure and per patient.
Results
In total, 75 examinations with a digital SOVC-assisted biliary stone treatment, performed in 60 patients, were identified. Biliary stones were mainly located extrahepatic (64%) and less frequently intrahepatic (36%). The median stone size was 20 mm (interquartile range [IQR]: 10–25 mm) and the median stone number was 1 (IQR: 1–2). Digital SOVC-based treatment of biliary stone disease was successful in 95% of patients and 15% needed at least two treatment sessions. Evaluated per procedure, a complete stone removal was accomplished in 67% of all examinations (including initial and repeated procedures), while an incomplete stone removal was observed in 33% of cases. The per procedure analyzes revealed that the success rates for a complete stone removal were similar between LL and EHL (66% vs. 68%; p = 0.87). Complications, such as postinterventional cholangitis and pancreatitis occurred in 16% of examinations; however, except from one case, all were mild or moderate and no procedure-associated mortality occurred.
Conclusions
Digital SOVC-assisted biliary stone treatment is highly effective even in cases with difficult biliary stones and might be considered the new standard of care for these patients. Furthermore, mild up to moderate complications were intermittently observed which might document the complexity of our included cases.



Similar content being viewed by others
References
Williams E, Beckingham I, El Sayed G, Gurusamy K, Sturgess R, Webster G, Young T (2017) Updated guideline on the management of common bile duct stones (CBDS). Gut 66:765–782
Qiu Y, Yang Z, Li Z, Zhang W, Xue D (2015) Is preoperative MRCP necessary for patients with gallstones? An analysis of the factors related to missed diagnosis of choledocholithiasis by preoperative ultrasound. BMC Gastroenterol 15:158
European Association for the Study of the Liver. Electronic address EEE (2016) EASL clinical practice guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol 65:146–181
Baron TH, Harewood GC (2004) Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol 99:1455–1460
Vlavianos P, Chopra K, Mandalia S, Anderson M, Thompson J, Westaby D (2003) Endoscopic balloon dilatation versus endoscopic sphincterotomy for the removal of bile duct stones: a prospective randomised trial. Gut 52:1165–1169
Tringali A, Lemmers A, Meves V, Terheggen G, Pohl J, Manfredi G, Hafner M, Costamagna G, Deviere J, Neuhaus H, Caillol F, Giovannini M, Hassan C, Dumonceau JM (2015) Intraductal biliopancreatic imaging: European Society of Gastrointestinal Endoscopy (ESGE) technology review. Endoscopy 47:739–753
Pereira P, Peixoto A, Andrade P, Macedo G (2017) Peroral cholangiopancreatoscopy with the SpyGlass(R) system: what do we know 10 years later. J Gastrointestin Liver Dis 26:165–170
Shah RJ, Neuhaus H, Parsi M, Reddy DN, Pleskow DK (2018) Randomized study of digital single-operator cholangioscope compared to fiberoptic single-operator cholangioscope in a novel cholangioscopy bench model. Endosc Int Open 6:E851–E856
Bokemeyer A, Gross D, Bruckner M, Nowacki T, Bettenworth D, Schmidt H, Heinzow H, Kabar I, Ullerich H, Lenze F (2019) Digital single-operator cholangioscopy: a useful tool for selective guidewire placements across complex biliary strictures. Surg Endosc 33:731–737
Lenze F, Bokemeyer A, Gross D, Nowacki T, Bettenworth D, Ullerich H (2018) Safety, diagnostic accuracy and therapeutic efficacy of digital single-operator cholangioscopy. United European Gastroenterol J 6(6):902–909
Imanishi M, Ogura T, Kurisu Y, Onda S, Takagi W, Okuda A, Miyano A, Amano M, Nishioka N, Masuda D, Higuchi K (2017) A feasibility study of digital single-operator cholangioscopy for diagnostic and therapeutic procedure (with videos). Medicine (Baltimore) 96:e6619
Ogura T, Imanishi M, Kurisu Y, Onda S, Sano T, Takagi W, Okuda A, Miyano A, Amano M, Nishioka N, Yamada T, Masuda D, Takenaka M, Kitano M, Higuchi K (2017) Prospective evaluation of digital single-operator cholangioscope for diagnostic and therapeutic procedures (with videos). Dig Endosc 29(7):782–789
Navaneethan U, Hasan MK, Kommaraju K, Zhu X, Hebert-Magee S, Hawes RH, Vargo JJ, Varadarajulu S, Parsi MA (2016) Digital, single-operator cholangiopancreatoscopy in the diagnosis and management of pancreatobiliary disorders: a multicenter clinical experience (with video). Gastrointest Endosc 84:649–655
Kamiyama R, Ogura T, Okuda A, Miyano A, Nishioka N, Imanishi M, Takagi W, Higuchi K (2018) Electrohydraulic lithotripsy for difficult bile duct stones under endoscopic retrograde cholangiopancreatography and peroral transluminal cholangioscopy guidance. Gut Liver 12:457–462
Brewer Gutierrez OI, Bekkali NLH, Raijman I, Sturgess R, Sejpal DV, Aridi HD, Sherman S, Shah RJ, Kwon RS, Buxbaum JL, Zulli C, Wassef W, Adler DG, Kushnir V, Wang AY, Krishnan K, Kaul V, Tzimas D, DiMaio CJ, Ho S, Petersen B, Moon JH, Elmunzer BJ, Webster GJM, Chen YI, Dwyer LK, Inamdar S, Patrick VB, Attwell A, Hosmer A, Ko C, Maurano A, Sarkar A, Taylor LJ, Gregory MH, Strand DS, Raza A, Kothari S, Harris JP, Kumta NA, Manvar A, Topazian MD, Lee YN, Spiceland CM, Trindade AJ, Bukhari MA, Sanaei O, Ngamruengphong S, Khashab MA (2018) Efficacy and safety of digital single-operator cholangioscopy for difficult biliary stones. Clin Gastroenterol Hepatol 16(918–926):e911
Turowski F, Hugle U, Dormann A, Bechtler M, Jakobs R, Gottschalk U, Notzel E, Hartmann D, Lorenz A, Kolligs F, Veltzke-Schlieker W, Adler A, Becker O, Wiedenmann B, Burgel N, Troger H, Schumann M, Daum S, Siegmund B, Bojarski C (2018) Diagnostic and therapeutic single-operator cholangiopancreatoscopy with SpyGlassDS: results of a multicenter retrospective cohort study. Surg Endosc 32(9):3981–3988
Wong JC, Tang RS, Teoh AY, Sung JJ, Lau JY (2017) Efficacy and safety of novel digital single-operator peroral cholangioscopy-guided laser lithotripsy for complicated biliary stones. Endosc Int Open 5:E54–E58
Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A (1998) Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 48:1–10
Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, Deal SE, Hoffinan B, Jacobson BC, Petrini JL, Safdi MA, Faigel DO, Pike IM, Endoscopy AAToQi (2006) Quality indicators for endoscopic retrograde cholangiopancreatography. Am J Gastroenterol 101:892–897
Committee AT, Watson RR, Parsi MA, Aslanian HR, Goodman AJ, Lichtenstein DR, Melson J, Navaneethan U, Pannala R, Sethi A, Sullivan SA, Thosani NC, Trikudanathan G, Trindade AJ, Maple JT (2018) Biliary and pancreatic lithotripsy devices. VideoGIE 3:329–338
Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N (1991) Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 37:383–393
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
Committee ASoP, Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM (2017) Adverse events associated with ERCP. Gastrointest Endosc 85:32–47
http://statpages.info/ctab2x2.html (2018) 2-way contingency table analysis
Lenze F, Nowacki TM, Beyna T, Ullerich H (2017) Direct peroral cholangioscopy with a new anchoring technique using the guide probe of Kautz: first clinical experiences. Endoscopy 49:909–912
Beyna T, Farnik H, Sarrazin C, Gerges C, Neuhaus H, Albert JG (2016) Direct retrograde cholangioscopy with a new prototype double-bending cholangioscope. Endoscopy 48:929–933
Beyna T, Schneider M, Pullmann D, Gerges C, Kandler J, Neuhaus H (2018) Motorized spiral colonoscopy: a first single-center feasibility trial. Endoscopy 50:518–523
Trikudanathan G, Arain MA, Attam R, Freeman ML (2014) Advances in the endoscopic management of common bile duct stones. Nat Rev Gastroenterol Hepatol 11:535–544
Kuo YT, Wang HP, Chang CY, Leung JW, Chen JH, Tsai MC, Liao WC (2017) Comparable long-term outcomes of 1-minute vs 5-minute endoscopic papillary balloon dilation for bile duct stones. Clin Gastroenterol Hepatol 15:1768–1775
Yang D, Buscaglia JM (2018) Digital single-operator cholangioscopy for difficult bile duct stones: out with the old in with the new? Clin Gastroenterol Hepatol 16:819–820
Deprez PH, Garces Duran R, Moreels T, Furneri G, Demma F, Verbeke L, Van der Merwe SW, Laleman W (2018) The economic impact of using single-operator cholangioscopy for the treatment of difficult bile duct stones and diagnosis of indeterminate bile duct strictures. Endoscopy 50:109–118
Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R (2007) Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 102:1781–1788
Laleman W, Verraes K, Van Steenbergen W, Cassiman D, Nevens F, Van der Merwe S, Verslype C (2017) Usefulness of the single-operator cholangioscopy system SpyGlass in biliary disease: a single-center prospective cohort study and aggregated review. Surg Endosc 31:2223–2232
Ding X, Zhang F, Wang Y (2015) Risk factors for post-ERCP pancreatitis: a systematic review and meta-analysis. Surgeon 13:218–229
Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE (2019) Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 51:472–491
Teoh AY, Cheung FK, Hu B, Pan YM, Lai LH, Chiu PW, Wong SK, Chan FK, Lau JY (2013) Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology 144:341–345
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Diana Lang and Drs. Arne Bokemeyer, Christian Gerges, Iyad Kabar and Frank Lenze as well as Prof. Dr. Dominik Bettenworth and Prof. Dr. Hartmut Schmidt have no conflicts of interest or financial ties to disclose. The following authors disclosed financial relationships relevant to this manuscript: Dr. Hansjoerg Ullerich received honoraria for lectures from Falk Foundation; Dr. Torsten Beyna received honoraria for consultancy and lectures from Boston Scientific and Olympus; Prof. Dr. Horst Neuhaus received honoraria for consultancy and lectures from Boston Scientific and Olympus.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bokemeyer, A., Gerges, C., Lang, D. et al. Digital single-operator video cholangioscopy in treating refractory biliary stones: a multicenter observational study. Surg Endosc 34, 1914–1922 (2020). https://doi.org/10.1007/s00464-019-06962-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06962-0