Abstract
Background
There is a lack of consensus on the continuation or cessation of perioperative antiplatelet and anticoagulation therapies in inguinal hernia repair, therefore, the local hospital protocols dealing with these agents vary. The aim of this study is to investigate the risk and safety of perioperative antiplatelet and anticoagulation therapies in patients undergoing elective inguinal hernia repair.
Methods
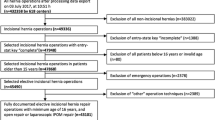
The major databases (PubMed, Embase, Springer, and Cochrane Library) were searched, and all studies published through January 2019 were identified, using the keywords Aspirin, Clopidogrel, Warfarin, antiplatelet, anticoagulation, inguinal hernia repair, bleeding, hematoma, complications. All relevant articles and reference lists in these original studies were also obtained from the above databases.
Results
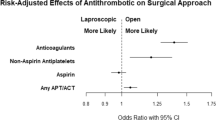
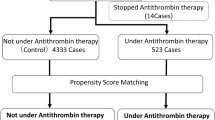
Thirteen articles were identified, ten studies reported the results of perioperative application of antiplatelet therapy during inguinal hernia repair, nine trials reported the outcomes perioperative use of anticoagulation therapy in inguinal hernia repair, and six articles reported the results of both agents. One study did not indicate the perioperative cessation or continuation of the corresponding agents. Cessation of antiplatelets was reported in three studies and continuation of antiplatelets was used in six studies, they all demonstrated similar incidence of the bleeding complications, as compared with controls. Continued perioperative anticoagulation with Warfarin was reported in six studies and Warfarin discontinuation 3 days prior to operation was examined in two studies, both reported similar postoperative bleeding-related complication rates providing international normalized ratio (INR) < 3, and the postoperative hematoma incidence increased in the condition of INR > 3.
Conclusion
Our results indicated that, for both open and laparoscopic inguinal hernia repair, there is no need to stop the antiplatelet therapy (Aspirin or Clopidogrel), and due to the limited evidence and the complexity of each patient’ condition, the continuation or cessation of anticoagulation with Warfarin should be tailored on a case-by-case basis.

Similar content being viewed by others
References
Cruden NLM, Harding SA, Flapan AD, Graham C, Wild SH, Slack R, Pell JP, Newby DE, on behalf of the Scottish Coronary Revascularisation Register Steering Committee (2010) Previous coronary stent implantation and cardiac events in patients undergoing noncardiac surgery. Circ Cardiovasc Interv 3:236–242
Anwaruddin S, Askari AT, Saudye H, Batizy L, Houghtaling PL, Alamoudi M, Militello M, Muhammad K, Kapadia S, Ellis SG (2009) Characterization of post-operative risk associated with priordrug-eluting stent use. JACC Cardiovasc Interv 2:542–549
Chu EW, Chernoguz A, Divino CM (2016) The evaluation of clopidogrel use in perioperative general surgery patients: a prospective randomized controlled trial. Am J Surg 211(6):1019–1025
Chu EW, Telem DA, Chernoguz A, Divino CM (2011) Assessing the risk of clopidogrel-related bleeding complications in patients undergoing inguinalherniorrhaphy. Hernia 15(1):31–35
Antolovic D, Rakow A, Contin P, Ulrich A, Rahbari NN, Büchler MW, Weitz J, Koch M (2012) A randomised controlled pilot trial to evaluate and optimize the use of anti-platelet agents in the perioperative management in patients undergoing general and abdominal surgery–the APAP trial (ISRCTN45810007). Langenbecks Arch Surg 397(2):297–306
Ong W, Shen T, Tan WB, Lomanto D (2016) Is preoperative withdrawal of aspirin necessary in patients undergoing elective inguinal herniarepair? Surg Endosc 30(12):5542–5549
McLemore EC, Harold KL, Cha SS, Johnson DJ, Fowl RJ (2006) The safety of open inguinal herniorraphy in patients on chronic warfarin therapy. Am J Surg 192(6):860–864
Wakasugi M, Akamatsu H, Yoshidome K, Tori M, Ueshima S, Omori T, Tei M, Masuzawa T, Iwamoto T, Nishida T (2013) Totally extraperitoneal inguinal hernia repair in patients on antithrombotic therapy: a retrospective analysis. Surg Today 43(8):942–945
Köckerling F, Roessing C, Adolf D, Schug-Pass C, Jacob D (2016) Has endoscopic (TEP, TAPP) or open inguinal hernia repair a higher risk of bleeding in patients with coagulopathy or antithrombotic therapy? Data from the Herniamed Registry. Surg Endosc 30(5):2073–2081
Poldermans D, Bax JJ, Boersma E, De Hert S, Eeckhout E, Fowkes G, Gorenek B, Hennerici MG, Lung B, Kelm M, Kjeldsen KP, Kristensen SD, Lopez-Sendon J, Pelosi P, Philippe F, Pierard L, Ponikowski P, Schmid JP, Sellevold OF, Sicari R, Van den Berghe G, Vermassen F, Hoeks SE, Vanhorebeek I, ESC Committee for Practice Guidelines (2009) Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery: the Task Force for Preoperative Cardiac Risk Assessment and Perioperative Cardiac Management in Noncardiac Surgery of the European Society of Cardiology (ESC) and European Society of Anaesthesiology (ESA). Eur Heart J 30(22):2769–2812
Douketis JD, Berger PB, Dunn AS, JaVer AK, Spyropoulos AC, Becker RC, Ansell J, American College of Chest Physicians (2008) The perioperative management of antithrombotic therapy: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 133(6 Suppl):299S–339S
Mahla ELT, Vicenzi MN, Werkgartner G, Maier R, Probst C, Metzler H (2001) Thromboelastography for monitoring prolonged hypercoagulability after major abdominal surgery. Anesth Analg 92(3):572–577
Samama CM, Thiry D, Elalamy I, Diaby M, Guillosson J-J, Kieffer E, Coriat P (2001) Perioperative activation of hemostasis in vascular surgery patients. Anesthesiology 94(1):74–78
Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, Airoldi F, Chieffo A, Montorfano M, Carlino M, Michev I, Corvaja N, Briguori C, Gerckens U, Grube E, Colombo A (2005) Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 293(17):2126–2130
Van Werkum JW, Heestermans AA, Zomer AC, Kelder JC, Suttorp MJ, Rensing BJ, Koolen JJ, Brueren BR, Dambrink JH, Hautvast RW, Verheugt FW, ten Berg JM (2009) Predictors of coronary stent thrombosis: the Dutch Stent Thrombosis Registry. J Am Coll Cardiol 53(16):1399–1409
Ferreira-González I, Marsal JR, Ribera A, Permanyer-Miralda G, García-Del Blanco B, Martí G, Cascant P, Martín-Yuste V, Brugaletta S, Sabaté M, Alfonso F, Capote ML, De La Torre JM, Ruíz-Lera M, Sanmiguel D, Cárdenas M, Pujol B, Baz JA, Iñiguez A, Trillo R, González-Béjar O, Casanova J, Sánchez-Gila J, García-Dorado D (2010) Background, incidence, and predictors of antiplatelet therapy discontinuation during the first year after drug-eluting stent implantation. Circulation 122(10):1017–1025
Kearon C, Hirsh J (1997) Management of anticoagulation before and after elective surgery. N Engl J Med 336:1506–1511
Beving H, Zhao C, Albage A, Ivert T (1996) Abnormally high platelet activity after discontinuation of acetylsalicylic acid treatment. Blood Coagul Fibrinolysis 7:80–84
Biondi-Zoccai GG, Lotrionte M, Agostoni P, Abbate A, Fusaro M, Burzotta F, Testa L, Sheiban I, Sangiorgi G (2006) A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease. Eur Heart J 27:2667–2674
Smoot RL, Oderich GS, Taner CB, Greenlee SM, Larson DR, Cragun EB, Farley DR (2008) Postoperative hematoma following inguinal herniorrhaphy: patient characteristics leading to increased risk. Hernia 12(3):261–265
Zeb MH, Pandian TK, El Khatib MM, Naik ND, Chandra A, Morris DS, Smoot RL, Farley DR (2016) Risk factors for postoperative hematoma after inguinal hernia repair: an update. J Surg Res 205(1):33–37
Sanders DL, Shahid MK, Ahlijah B, Raitt JE, Kingsnorth AN (2008) Inguinal hernia repair in the anticoagulated patient: a retrospective analysis. Hernia 12(6):589–592
Stucky CC, Garvey EM, Johnson DJ, Chapital AB, Gossage CM, Wasif N, Harold KL (2015) Challenging a surgical dictum: results from a 10-year experience on the safety of open inguinal herniorrhaphy in patients on chronic warfarin therapy. Hernia 19(1):83–87
Wakasugi M, Tei M, Suzuki Y, Furukawa K, Masuzawa T, Kishi K, Tanemura M, Akamatsu H (2017) Single-incision totally extraperitoneal inguinal hernia repair is feasible and safe in patients on antithrombotic therapy: a single-center experience of 92 procedures. Asian J Endosc Surg. 10(3):301–307
Ho CH, Wu CC, Wu CC, Tsai YC (2018) Laparoscopic total extraperitoneal inguinal hernia repair is safe and feasible in patients with continuation of antithrombotics. Minim Access Surg. https://doi.org/10.4103/jmas.jmas_128_18
Ferraris VA, Ferraris SP, Moliterno DJ, Camp P, Walenga JM, Messmore HL, Jeske WP, Edwards FH, Royston D, Shahian DM, Peterson E, Bridges CR, Despotis G; Society of Thoracic Surgeons (2005) The Society of Thoracic Surgeons practice guideline series: aspirin and other antiplatelet agents during operative coronary revascularization (executive summary). Ann Thorac Surg 79(4):1454–1461
Wolf AM, Pucci MJ, Gabale SD, McIntyre CA, Irizarry AM, Kennedy EP, Rosato EL, Lavu H, Winter JM, Yeo CJ (2014) Safety of perioperative aspirin therapy in pancreatic operations. Surgery 155:39–46
Oscarsson A, Gupta A, Fredrikson M, Jarhult J, Nystrom M, Pettersson E, Darvish B, Krook H, Swahn E, Eintrei C (2010) To continue or discontinue aspirin in the perioperative period: a randomized, controlled clinical trial. Br J Anaesth 104:305–312
Kaluza GL, Joseph J, Lee JR, Raizner ME, Raizner AE (2000) Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol 35:1288–1294
Vicenzi MN, Meislitzer T, Heitzinger B, Halaj M, Fleisher LA, Metzler H (2006) Coronary artery stenting and non-cardiac surgery—a prospective outcome study. Br J Anaesth 96:686–693
Collet JP, Montalescot G, Blanchet B, Tanguy ML, Golmard JL, Choussat R, Beygui F, Payot L, Vignolles N, Metzger JP et al (2004) Impact of prior use or recent withdrawal of oral antiplateletagents on acute coronary syndromes. Circulation 110(16):2361–2367
Maulaz AB, Bezerra DC, Michel P, Bogousslavsky J (2005) Effect of discontinuing aspirin therapy on the risk of brain ischemic stroke. Arch Neurol 62(8):1217–1220
ACC/AHA (2004) Guideline update for coronary artery bypass graft surgery. Circulation 110(14):e340–e437
Chassot P-G, Delabays A, Spahn DR (2007) Perioperative antiplatelet therapy: the case for continuing therapy in patients at risk of myocardial infarction. Br J Anaesth 99(3):316–328
Burger W, Chemnitius JM, Kneissl GD, Rücker G (2005) Lowdose aspirin for secondary cardiovascular prevention—cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation—review and meta-analysis. J Intern Med 257(5):399–414
Thachil J, Gatt A, Martlew V (2008) Management of surgical patients receiving anticoagulation and antiplatelet agents. Br J Surg 95(12):1437–1448
Spyropouos AC, Turpie AGG (2005) Perioperative bridging interruption with heparin for the patient receiving long-term anticoagulation. Curr Opin Pulm Med 11:373–379
Devereaux PJ, Mrkobrada M, Sessler DI, Leslie K, Alonso-Coello P, Kurz A, Villar JC, Sigamani A, Biccard BM, Meyhoff CS, Parlow JL, Guyatt G, Robinson A, Garg AX, Rodseth RN, Botto F, Lurati Buse G, Xavier D, Chan MT, Tiboni M, Cook D, Kumar PA, Forget P, Malaga G, Fleischmann E, Amir M, Eikelboom J, Mizera R, Torres D, Wang CY, VanHelder T, Paniagua P, Berwanger O, Srinathan S, Graham M, Pasin L, Le Manach Y, Gao P, Pogue J, Whitlock R, Lamy A, Kearon C, Baigent C, Chow C, Pettit S, Chrolavicius S, Yusuf S (2014) Aspirin in patients undergoing noncardiac surgery. N Engl J Med 370(16):1494–1503
Lundstro¨m KJ, Sandblom G, Smedberg S, Nordin P (2012) Risk factors for complications in groin hernia surgery: a national register study. Ann Surg 255(4):784–788
Ginelliová A, Farkaš D, Farkašová Iannaccone S, Vyhnálková V (2016) Unexpected fatal outcome of laparoscopic inguinal hernia repair. Forensic Sci Med Pathol 12(2):178–180
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Junsheng Li, Minggang Wang, and Tao Cheng have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, J., Wang, M. & Cheng, T. The safe and risk assessment of perioperative antiplatelet and anticoagulation therapy in inguinal hernia repair, a systematic review. Surg Endosc 33, 3165–3176 (2019). https://doi.org/10.1007/s00464-019-06956-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06956-y