Abstract
Introduction
Post-operative non-urgent hospital visits (NUR-HV) are an important quality target for reducing unnecessary healthcare utilization. The primary objective of this study was to characterize 90-day post-operative hospital use and determine independent predictors for NUR-HV and urgent (UR)-HV after elective laparoscopic paraesophageal hernia repair (LPEHR) and Nissen Fundoplication (LNF).
Methods
Five hundred and sixty-two primary LPEHR and LNF patients were retrospectively reviewed at a single institution. Ninety-day NUR-HV and UR-HV were compared to patients without post-operative HV using baseline medical and demographic data, preoperative work-up (manometry, pH testing, disease-specific quality of life and symptom scale scores (GERSS), and hospital course. Multiple logistic models were created using univariate associations (p < 0.1) to model independent predictors of NUR-HV and UR-HV.
Results
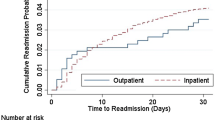
NUR-HV accounted for 52% (n = 30) of all 90-HV, while the remaining were UR-HV (n = 28, 48.3%). Compared to controls, NUR-HV were younger (51.2 ± 16.8 years vs. 57.6 ± 15.2, p = 0.05), had a lower baseline BMI (28.2 ± 6.4 vs. 31.3 ± 5.4, p = 0.003) and ASA scores (p = 0.02), presented with higher GERSS (46 (28–60) vs. 35 (19–48), p = 0.02) and dysphagia scores (3 (1–5) vs. 2 (0–4), p = 0.02), were associated with LNF (77.7% vs. 54.6%, p = 0.02), and experienced more post-operative dysphagia (13.3% vs. 4.6%, p = 0.06). UR-HV were older (64.0 ± 13.2 vs. 57.6 ± 15.2, p = 0.03), associated with LPEHR (67.9% vs. 45.4%, p = 0.02), longer hospital stay (2 (1–3) vs. 1 (1–2), p = 0.003), and increased overall (39.3% vs. 15.1%, p = 0.001) and urgent complications (34.6% vs. 8.3%, p < 0.005). Positive predictors of NUR-HV included ASA score < 3 (OR 4.4, p = 0.02), increasing GERSS (1.04, p = 0.01), and reduced peristalsis (OR 4.7, p = 0.01), while UR-HV were independently predicted by urgent complications (5.0, p < 0.00005).
Conclusions
NUR-HV accounted for half of post-operative visits following LNF/LPEHR and were predicted by distinct characteristics compared to UR-HV. This stratification provides novel insight that will guide both preoperative counseling and post-operative quality initiatives.

Similar content being viewed by others
References
Jencks SF, Williams MV, Coleman EA (2009) Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 360(14):1418–1428
Chen J et al (2017) Preventing Returns to the Emergency Department FollowingBariatric Surgery. Obes Surg 27(8):1986–1992
Celio AC, Kasten KR, Pofahl WE, Pories WJ, Spaniolas K (2016) Causes of readmission after laparoscopic and open ventral hernia repair: identifying failed discharges and opportunities for action. Surgery 160(2):413–417
Kripalani S, Theobald CN, Anctil B, Vasilevskis EE (2014) Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med 65(1):471–485
Molina JC et al (2018) Same day discharge for benign laparoscopic hiatal surgery: a feasibility analysis. Surg Endosc 32(2):937–944
Petrick A, Brindle SA, Vogels E, Dove J, Parker D, Gabrielsen J (2018) The readmission contradiction: toward clarifying common misconceptions about bariatric readmissions and quality improvement. Surg Obes Relat Dis 14(7):1026–1032
Poupore AK, Stem M, Molena D, Lidor AO (2016) Incidence, reasons, and risk factors for readmission after surgery for benign distal esophageal disease. Surgery 160(3):599–606
Rosero EB, Joshi GP (2017) Hospital readmission after ambulatory laparoscopic cholecystectomy: incidence and predictors. J Surg Res 219:108–115
Jalilvand A, Dewire J, Detty A, Needleman B, Noria S (2018) Baseline psychiatric diagnoses are associated with early readmissions and long hospital length of stay after bariatric surgery. Surg Endosc 33(5):1661–1666
Jalilvand A et al (2016) Impact of care coaching on hospital length of stay, readmission rates, postdischarge phone calls, and patient satisfaction after bariatric surgery. Surg Obes Relat Dis 12(9):1737–1745
Reyes-Pérez A, Sánchez-Aguilar H, Velázquez-Fernández D, Rodríguez-Ortíz D, Mosti M, Herrera MF (2016) Analysis of causes and risk factors for hospital readmission after Roux-en-Y gastric bypass. Obes Surg 26(2):257–260
Hong B, Stanley E, Reinhardt S, Panther K, Garren MJ, Gould JC (2012) Factors associated with readmission after laparoscopic gastric bypass surgery. Surg Obes Relat Dis 8(6):691–695
Funk LM, Suzo A, Mikami DJ, Needleman BJ (2014) Two-year outcomes for medicaid patients undergoing laparoscopic Roux-en-Y gastric bypass: a case-control study. Obes Surg 24(10):1679–1685
Mora-Pinzon MC et al (2017) Emergency department visits and readmissions within 1 year of bariatric surgery: a statewide analysis using hospital discharge records. Surgery 162(5):1155–1162
Chimukangara M, Frelich MJ, Bosler ME, Rein LE, Szabo A, Gould JC (2016) The impact of frailty on outcomes of paraesophageal hernia repair. J Surg Res 202(2):259–266
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Anahita D Jalilvand ,Kyle A Perry ,Patricia Belle,and Monet McNally have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jalilvand, A.D., McNally, M., Belle, P. et al. Patterns of hospital utilization after elective minimally invasive foregut surgery. Surg Endosc 34, 2149–2157 (2020). https://doi.org/10.1007/s00464-019-06953-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06953-1