Abstract
Background
Achalasia outcome is primarily defined using the Eckardt score with failure recognized as > 3. However, patients experience many changes after myotomy including new onset GERD, swallowing difficulties, and potential need for additional treatment. We aim to devise a comprehensive assessment tool to demonstrate the extent of patient-reported outcomes, objective changes, and need for re-interventions following myotomy.
Methods
We performed a retrospective chart review of surgically treated primary achalasia patients. We identified 185 patients without prior foregut surgery who underwent either per oral endoscopic myotomy (POEM) or Heller myotomy from 2005 to 2017. Eight outcome measures in subjective, objective, and interventional categories formulated a global postoperative assessment tool. These outcomes included Eckardt score, Dakkak Dysphagia score, GERD–HRQL score, normalization of pH scores and IRP, esophagitis, timed barium clearance at 5 min, and the most invasive re-intervention performed.
Results
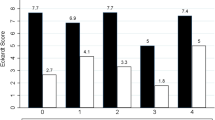
Of 185 patients, achalasia subtypes included Type I = 42 (23%), II = 109 (59%), and III = 34 (18%). Patients underwent minimally invasive myotomy in 114 (62%), POEM in 71 (38%). Median proximal myotomy length was 4 cm (IQR 4–5) and distal 2 cm (IQR 2–2.5). Based on postoperative Eckardt score, 135/145 (93%) had successful treatment of achalasia. But, only 47/104 (45%) reported normal swallowing, and 78/108 (72%) had GERD–HRQL score ≤ 10. Objectively, IRP was normalized in 48/60 (80%), whereas timed barium clearance occurred in 51/84 (61%). No evidence of esophagitis was documented in 82/115 (71%). Postoperative normal DeMeester scores occurred in 38/76 (50%). No additional treatments were required in 110/139 (79%) of patients.
Conclusions
Use of the Eckardt score alone to assess outcomes after achalasia surgery shows outstanding results. Using patient-reported outcomes, objective measurements, re-intervention rates, organized into a report card provides a more comprehensive and informative view.

Similar content being viewed by others
References
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet 383(9911):83–93
Zaninotto G, Bennett C, Boeckxstaens G, Costantini M, Ferguson MK, Pandolfino JE, Patti MG, Ribeiro U, Richter J, Swanstrom L, Tack J, Triadafilopoulos G, Markar SR, Salvador R, Faccio L, Andreollo NA, Cecconello I, Costamagna G, da Rocha JRM, Hungness ES, Fisichella PM, Fuchs KH, Gockel I, Gurski R, Gyawali CP, Herbella FAM, Holloway RH, Hongo M, Jobe BA, Kahrilas PJ, Katzka DA, Dua KS, Liu D, Moonen A, Nasi A, Pasricha PJ, Penagini R, Perretta S, Sallum RAA, Sarnelli G, Savarin EO, Schlottmann F, Sifrim D, Soper N, Tatum RP, Vaezi MF, van Herwaarden-Lindeboom M, Vanuytsel T, Vela MF, Watson DI, Zerbib F, Gittens S, Pontillo C, Vermigli S, Inama D, Low DE (2018) The 2018 ISDE achalasia guidelines. Dis Esophagus 31:1–29
Eckardt VF, Aignherr C, Bernhard G (1992) Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology 103:1732–1738
Martinek J, Svecova H, Vackova Z, Radek D, Ngo O, Krajciova J, Kieslichova E, Janousek R, Pazdro A, Harustiak T, Zdrhova L, Loudova P, Stirand P, Spicak J (2018) Per-oral endoscopic myotomy (POEM): mid-term efficacy and safety. Surg Endosc 32(3):1293–1302
Boeckxstaens GE, Annese V, Bruley des Varannes S, Chaussade S, Costantini M, Cuttitta A, Ilizalde I, Fumagalli U, Gaudric M, Rohof WO, Smouth AJ, Tack J, Zwinderman AH, Zaninotto G, Busch OR, for the European Achalasia Trial Investigators (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364(19):1807–1816
Raja S, Schraufnagel DP, Blackstone EH, Murthy SC, Thota PN, Thuita L, Lopez R, Gabbard SL, Ray MN, Wadhwa N, Sanaka M, Zanoni A, Rice TW (2019) Reintervention after Heller myotomy for achalasia: is it inevitable? Ann Thorac Surg 107(3):860–867
Louie BE, Schneider AM, Schembre DB, Aye RW (2017) Impact of prior interventions on outcomes during per oral endoscopic myotomy. Surg Endosc 31(4):1841–1848
Greene CL, Chang EJ, Oh DS, Worrell SG, Hagen JA, DeMeester SR (2015) High resolution manometry sub-classification of achalasia; does it really matter? Surg Endosc 29:1363–1367
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, Pandolfino JE, International High Resolution Manometry Working Group (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27(2):160–174
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20(2):130–134
Dakkak M, Bennett JR (1992) A new dysphagia score with objective validation. J Clin Gastroenterol 14(2):99–100
Armstrong D, Bennett JR, Blum AL, Dent J, De Dombal FT, Galmiche JP, Lundell L, Margulies M, Richter JE, Spechler SJ, Tytgat GNJ, Wallin L (1996) The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology 111(1):85–92
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259(6):1098–1103
Ferri LE, Cools-Lartigue J, Cao J, Miller L, Mayrand S, Fried GM, Darling G (2010) Clinical predictors of achalasia. Dis Esophagus 23(1):76–81
Urbach DR, Tomlinson GA, Harnish JL, Martino R, Diamant NE (2005) A measure of disease-specific health-related quality of life for achalasia. Am J Gastroenterol 100(8):1668–1676
Kachala SS, Rice TW, Baker ME, Rajeswaran J, Thota PN, Murthy SC, Blackstone EH, Zanoni A, Raja S (2018) Value of routine timed barium esophagram follow-up in achalasia after myotomy. J Thorac Cardiovasc Surg 156(2):871–877
Csendes A, Braghetto I, Burdiles P, Korn O, Csendes P, Henriquez A (2006) Very late results of esophagomyotomy for patients with achalasia. Ann Surg 243(2):196–203
Gossage JA, Devitt PG, Watson DI, Myers JC, Jamieson GG, Thompson SK (2014) Surveillance endoscopy at five or more years after cardiomyotomy for achalasia. Ann Surg 259:464–468
Tassi V, Lugaresi M, Daddi N, Mattioli S (2019) On the sequence gastro-esophageal reflux, esophagitis, Barrett’s esophagus, dysplasia, adenocarcinoma after Heller myotomy for the surgical therapy of esophageal achalasia [abstract]. In: 27th European Conference on General Thoracic Surgery, 2019, June 9-12; Dublin, Ireland: ESTS; 2019. Abstract nr O-054
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Brian E. Louie receives educational grants from Boston Scientific, ERBE, and Olympus. Drs. Ralph W. Aye, Alexander S. Farivar, Adam J. Bograd, and Ealaf Shemmeri have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shemmeri, E., Aye, R.W., Farivar, A.S. et al. Use of a report card to evaluate outcomes of achalasia surgery: beyond the Eckardt score. Surg Endosc 34, 1856–1862 (2020). https://doi.org/10.1007/s00464-019-06952-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06952-2