Abstract
Background
The majority of patients who undergo a laparoscopic fundoplication for gastroesophageal reflux disease (GERD) have a structural (hiatal hernia, shortened lower esophageal sphincter [LES]) or functional (weak LES) defect of the gastroesophageal junction (GEJ). We hypothesized that the symptomatic outcomes of fundoplication in patients with a competent GEJ prior to surgery are inferior to those with an incompetent GEJ.
Methods
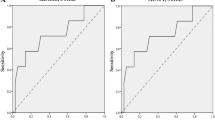
This is a retrospective review of prospectively maintained data on subjects who underwent primary laparoscopic fundoplication (Nissen or Toupet) for medically refractory and confirmed GERD. Three esophageal manometry variables were used to determine GEJ competency: (1) hiatal hernia (normal = no hernia), (2) total lower esophageal sphincter length (normal ≥ 2.43 cm), and (3) lower esophageal sphincter pressure (normal = 15.0–43.7 mmHg). Patients in the competent group had normal values for all 3 variables. Symptomatic outcomes were assessed with the GERD Health-Related Quality of Life (HRQL) survey administered pre- and postoperatively, and then compared both intragroup, intergroup, and by procedure.
Results
A total of 78 patients met inclusion criteria—17 competent GEJ and 61 incompetent GEJ patients. GERD-HRQL scores improved in the incompetent cohort at all intervals out to 2 years postoperatively. GERD-HRQL improved in the competent cohort at 2 months, with no difference at 6 months or 2 years postoperatively compared to preoperative scores. Competent GEJ patients receiving a Nissen fundoplication had a higher rate of additional procedures (endoscopy with or without dilation, pH studies) following surgery to address recurrent or persistent GERD symptoms compared to Toupet.
Conclusions
GERD patients with a competent GEJ report a lower GERD-HRQL with more frequent and severe reflux symptoms up to 2 years post-fundoplication. Competent GEJ patients receiving a Nissen fundoplication are more likely to have additional procedures to address symptoms following surgery. Surgeons should approach patients with a competent GEJ and medically refractory GERD with caution.
Similar content being viewed by others
References
El-Serag HB, Sweet S, Winchester CC (2014) Dent J (2014) Update on the epidemiology of gastroesophageal reflux disease: a systematic review. Gut 63:871–880
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, Global Consensus Group (2006) The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 101:1900–1902
Rickenbacher N, Kötter T, Kochen MM, Scherer M, Blozik E (2014) Fundoplication versus medical management of gastroesophageal reflux disease: systematic review and meta-analysis. Surg Endosc 28:143–155
Herregods TV, Bredenoord AJ, Smout AJ (2015) Pathophysiology of gastroesophageal reflux disease: new understanding in a new era. Neurogastroenterol Motil 27:1202–1213
Zaninotto G, DeMeester TR, Schwizer W, Johansson KE, Cheng SC (1988) The lower esophageal sphincter in health and disease. Am J Surg 155:104–111
Tsuboi K, Hoshino M, Sundaram A, Yano F, Mittal SK (2012) Role of the lower esophageal sphincter on esophageal acid exposure—a review of over 2000 patients. Trop Gastroenterol 33(2):107–111
Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJPM (2013) Normal values for esophageal high-resolution manometry. Neurogastroenterol Motil 25:762-e579. https://doi.org/10.1111/nmo.12167
Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Shah N, Kahrilas PJ (2006) Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol 290:G988–G997. https://doi.org/10.1152/ajpgi.00510.2005
Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJPM (2011) Reproducibility of esophageal high-resolution manometry: reproducibility of esophageal HRM. Neurogastroenterol Motil 23:e271–e276. https://doi.org/10.1111/j.1365-2982.2011.01713.x
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20:130–134
Staehelin A, Zingg U, Devitt PG, Esterman AJ, Smith L, Jamieson GG, Watson DI (2014) Preoperative factors predicting clinical outcome following laparoscopic fundoplication. World J Surg 38(6):1431–1443
van Herwaarden MA, Samsom M, Smout AJ (2000) Excess gastroesophageal reflux in patients with hiatus hernia is caused by mechanisms other than transient LES relaxations. Gastroenterology 119:1439–1446
Patti MG, Goldberg HI, Arcerito M, Bortolasi L, Tong J, Way LW (1996) Hiatal hernia size affects lower esophageal sphincter function, esophageal acid exposure, and the degree of mucosal injury. Am J Surg 171:182–186
Jones MP, Sloan SS, Jovanovic B, Kahrilas PJ (2002) Impaired egress rather than increased access: an important independent predictor of erosive oesophagitis. Neurogastroenterol Motil 14:625–631
Mittal RK, Holloway RH, Penagini R, Blackshaw LA, Dent J (1995) Transient lower esophageal sphincter relaxation. Gastroenterology 109:601–610
Roman S, Holloway R, Keller J, Herbella F, Zerbib F, Xiao Y, Bernard L, Bredenoord AJ, Bruley des Varannes S, Chen M, Fox M, Kahrilas PJ, Mittal RK, Penagini R, Savarino E, Sifrim D, Wu J, Decullier E, Pandolfino JE, Mion F (2017) Validation of criteria for the definition of transient lower esophageal sphincter relaxations using high-resolution manometry. Neurogastroenterol Motil 29:e12920
Trudgill NJ, Riley SA (2001) Transient lower esophageal sphincter relaxations are no more frequent in patients with gastroesophageal reflux disease than in asymptomatic volunteers. Am J Gastroenterol 96:2569–2574
Sifrim D, Holloway R, Silny J, Tack J, Lerut A, Janssens J (2001) Composition of the postprandial refluxate in patients with gastroesophageal reflux disease. Am J Gastroenterol 96:647–655
Gyawali CP, Roman S, Bredenoord AJ, Fox M, Keller J, Pandolfino JE, Sifrim D, Tatum R, Yadlapati R, Savarino E, International GERD Consensus Working Group (2017) Classification of esophageal motor findings in gastro-esophageal reflux disease: conclusions from an international consensus group. Neurogastroenterol Motil 29:e13104
Lin S, Ke M, Xu J, Kahrilis PJ (1994) Impaired esophageal emptying in reflux disease. Am J Gastroenterol 89:1003–1006
Bredenoord AJ, Hemmink GJ, Smout AJ (2009) Relationship between gastroesophageal reflux pattern and severity of mucosal damage. Neurogastroenterol Motil 21:807–812
Smout A, Fox M (2012) Weak and absent peristalsis. Neurogastroeneterol Motil 24(suppl 1):40–47
Heider TR, Behrns KE, Koruda MJ, Shaheen NJ, Lucktong TA, Bradshaw B, Farrell TM (2003) Fundoplication improves disordered esophageal motility. J Gastrointest Surg 7:159–163
Fuchs HF, Gutschow CA, Brinkmann S, Herbold T, Bludau M, Schröder W, Bollschweiler E, Hölscher AH, Leers JM (2014) Effect of laparoscopic antireflux surgery on esophageal motility. Dig Surg 31(4–5):354–358. https://doi.org/10.1159/000368662
Gyawali CP, Kushnir VM (2011) High-resolution manometric characteristics help differentiate types of distal esophageal obstruction in patients with peristalsis. Neurogastroenterol Motil 23:502-e197
Weijenborg PW, Savarino E, Kessing BF, Roman S, Costantini M, Oors JM, Smout AJ, Bredenoord AJ (2015) Normal values of esophageal motility after antireflux surgery; a study using high-resolution manometry. Neurogastroenterol Motil 27:929–935
Shaker A, Stoikes N, Drapekin J, Kushnir V, Brunt LM, Gyawali CP (2013) Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol 108:1706–1712
Stoikes N, Drapekin J, Kushnir V, Shaker A, Brunt LM, Gyawali CP (2012) The value of multiple rapid swallows during preoperative esophageal manometry before laparoscopic antireflux surgery. Surg Endosc 26:3401–3407
Anderson JA, Myers JC, Watson DI, Gabb M, Mathew G, Jamieson GG (1998) Concurrent fluoroscopy and manometry reveal differences in laparoscopic Nissen and anterior fundoplication. Dig Dis Sci 43:847–853
DeHaan RK, Davila D, Frelich MJ, Gould JC (2017) Esophagogastric junction distensibility is greater following Toupet compared to Nissen fundoplication. Surg Endosc 31(1):193–198
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Gould is a consultant for Torax/Ethicon. Dr. Schumm, Mr. Turner, and Ms. Helm and Hetzelhave no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Turner, B., Helm, M., Hetzel, E. et al. The relationship between gastroesophageal junction integrity and symptomatic fundoplication outcomes. Surg Endosc 34, 1387–1392 (2020). https://doi.org/10.1007/s00464-019-06921-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06921-9