Abstract
Background
A growing body of evidence shows that experience and acquired skills from surrogate surgical procedures may be transferrable to a specific index operation. It is unclear whether this applies to bariatric surgery. This study aims to determine whether there is a surrogate volume effect of common laparoscopic general surgery procedures on all-cause bariatric surgical morbidity.
Methods
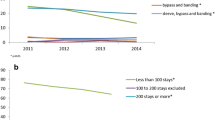
This was a population-based study of all patients aged ≥ 18 who received a bariatric procedure in Ontario from 2008 to 2015. The main outcome of interest was all-cause morbidity during the index admission. All-cause morbidity included any documented complication which extended length of stay by 24 h or required reoperation. Bariatric cases included laparoscopic Roux-en-Y gastric bypass, sleeve gastrectomy, and biliopancreatic diversion with duodenal switch. Non-bariatric cases included three common laparoscopic general surgery procedures.
Results
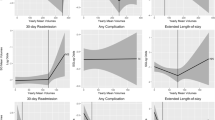
13,836 bariatric procedures were performed by 29 surgeons at nine centers of excellence. A reduction in all-cause morbidity was seen when bariatric surgeons exceeded 75 cases annually (OR 0.82, 95% CI 0.69–0.98, P = 0.023), with further reduction in increasing bariatric volume. However, the volume of non-bariatric surgeries did not significantly affect bariatric all-cause morbidity rates amongst bariatric surgeons, even when exceeding 100 cases (OR 0.84, 95% CI 0.61–1.12, P = 0.222).
Conclusions
The present study suggests that experience and skills acquired in performing non-bariatric laparoscopic general surgery does not appear to affect all-cause morbidity in bariatric surgery. Therefore, only a surgeon’s bariatric procedure volume should considered be a quality marker for outcomes after bariatric surgery.
Similar content being viewed by others
References
Chang S-H, Stoll CRT, Song J, Varela JE, Eagon CJ, Colditz GA (2014) The effectiveness and risks of bariatric surgery. JAMA Surg. 149:275. https://doi.org/10.1001/jamasurg.2013.3654
WHO (2015) Obesity. WHO, Geneva
Neff KJ, Olbers T, le Roux CW (2013) Bariatric surgery: the challenges with candidate selection, individualizing treatment and clinical outcomes. BMC Med 11:8. https://doi.org/10.1186/1741-7015-11-8
Morche J, Mathes T, Pieper D (2016) Relationship between surgeon volume and outcomes: a systematic review of systematic reviews. Syst Rev. https://doi.org/10.1186/s13643-016-0376-4
Surgeons AC (2016) Standards manual—resources for optimal care of the metabolic and bariatric surgery patient 2016. https://www.facs.org/~/media/files/qualityprograms/bariatric/mbsaqipstandardsmanual.ashx
Surgery AS for M and B (2018) Core curriculum for American Society for Metabolic and Bariatric Surgery—Fellowship Training Requirements. https://asmbs.org/app/uploads/2018/07/2018-Curriculum-Final.pdf
Shin RB (2005) Evaluation of the learning curve for laparoscopic Roux-en-Y gastric bypass surgery. Surg Obes Relat Dis. https://doi.org/10.1016/j.soard.2005.01.003
Stroh C, Köckerling F, Lange V, Wolff S, Knoll C, Bruns C, Manger T (2017) Does certification as bariatric surgery center and volume influence the outcome in rygb—data analysis of german bariatric surgery registry. Obes Surg. https://doi.org/10.1007/s11695-016-2340-8
Courcoulas AP, Yanovski SZ, Bonds D, Eggerman TL, Horlick M, Staten MA, Arterburn DE (2014) Long-term outcomes of bariatric surgery: a National Institutes of Health symposium. JAMA Surg 149:1323–1329. https://doi.org/10.1001/jamasurg.2014.2440
Weller WE, Rosati C, Hannan EL (2007) Relationship between surgeon and hospital volume and readmission after bariatric operation. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2006.12.031
Hollenbeak CS, Rogers AM, Barrus B, Wadiwala I, Cooney RN (2008) Surgical volume impacts bariatric surgery mortality: a case for centers of excellence. Surgery. https://doi.org/10.1016/j.surg.2008.05.013
Zevin B, Aggarwal R, Grantcharov TP (2012) Volume-outcome association in bariatric surgery: a systematic review. Ann Surg 256:60
Doumouras AG, Saleh F, Anvari S, Gmora S, Anvari M, Hong D (2017) Mastery in bariatric surgery: the long-term surgeon learning curve of Roux-en-Y gastric bypass. Ann Surg. https://doi.org/10.1097/sla.0000000000002180
Kohn GP, Galanko JA, Overby DW, Farrell TM (2010) High case volumes and surgical fellowships are associated with improved outcomes for bariatric surgery patients: a justification of current credentialing initiatives for practice and training. J Am Coll Surg 210:909–918. https://doi.org/10.1016/J.JAMCOLLSURG.2010.03.005
Modrall JG, Minter RM, Minhajuddin A, Eslava-Schmalbach J, Joshi GP, Patel S, Rosero EB (2017) The surgeon volume-outcome relationship. Ann Surg 267:1. https://doi.org/10.1097/SLA.0000000000002334
OBN (2015) OBN surgical task force recommendations
Smith MD, Patterson E, Wahed AS, Belle SH, Bessler M, Courcoulas AP, Flum D, Halpin V, Mitchell JE, Pomp A, Pories WJ, Wolfe B (2010) Relationship between surgeon volume and adverse outcomes after RYGB in longitudinal assessment of bariatric surgery (LABS) study. Surg Obes Relat Dis 6:118–125. https://doi.org/10.1016/j.soard.2009.09.009
Celio AC, Kasten KR, Brinkley J, Chung AY, Burruss MB, Pories WJ, Spaniolas K (2016) Effect of surgeon volume on sleeve gastrectomy outcomes. Obes Surg 26:2700–2704. https://doi.org/10.1007/s11695-016-2190-4
Nguyen NT, Paya M, Stevens CM, Mavandadi S, Zainabadi K, Wilson SE (2004) The relationship between hospital volume and outcome in bariatric surgery at academic medical centers. Trans Meet Am Surg Assoc CXXII:184–192. https://doi.org/10.1097/01.sla.0000140752.74893.24
Carbonell AM, Lincourt AE, Matthews BD, Kercher KW, Sing RF, Heniford BT (2005) National study of the effect of patient and hospital characteristics on bariatric surgery outcomes. Am Surg 71:308–314
Padwal R, Klarenbach S, Wiebe N, Hazel M, Birch D, Karmali S, Sharma AM, Manns B, Tonelli M (2011) Bariatric surgery: a systematic review of the clinical and economic evidence. J Gen Intern Med 26:1183–1194. https://doi.org/10.1007/s11606-011-1721-x
Courcoulas A, Schuchert M, Gatti G, Luketich J (2003) The relationship of surgeon and hospital volume to outcome after gastric bypass surgery in Pennsylvania: a 3-year summary. Surgery 134:613–621. https://doi.org/10.1016/S0039-6060(03)00306-4
Telem DA, Talamini M, Altieri M, Yang J, Zhang Q, Pryor AD (2015) The effect of national hospital accreditation in bariatric surgery on perioperative outcomes and long-term mortality. Surg Obes Relat Dis 11:749–757. https://doi.org/10.1016/j.soard.2014.05.012
Morton JM, Garg T, Nguyen N (2014) Does hospital accreditation impact bariatric surgery safety? Ann Surg 260:504–509. https://doi.org/10.1097/SLA.0000000000000891
Doumouras AG, Saleh F, Anvari S, Gmora S, Anvari M, Hong D (2018) Mastery in bariatric surgery. Ann Surg 267:489–494. https://doi.org/10.1097/SLA.0000000000002180
Doumouras AG, Saleh F, Anvari S, Gmora S, Anvari M, Hong D (2017) The effect of health system factors on outcomes and costs after bariatric surgery in a universal healthcare system: a national cohort study of bariatric surgery in Canada. Surg Endosc 31:4816–4823. https://doi.org/10.1007/s00464-017-5559-0
Sundbom M (2014) Laparoscopic revolution in bariatric surgery. World J Gastroenterol 20:15135–15143. https://doi.org/10.3748/wjg.v20.i41.15135
Urbach DR, Baxter NN (2004) Does it matter what a hospital is “high volume” for? specificity of hospital volume-outcome associations for surgical procedures: analysis of administrative data. BMJ 328:737–740. https://doi.org/10.1136/bmj.38030.642963.AE
Brethauer SA, Chand B, Schauer PR (2008) American Society for Metabolic and bariatric surgery (ASMBS) centers of excellence program. In: Nguyen N, Maria E, Ikramuddin S, Hutter M (eds) The SAGES manual: a practical guide to bariatric surgery. Springer, New York, pp 261–273
Ravesloot MJL, van Maanen JP, Hilgevoord AAJ, van Wagensveld BA, de Vries N (2012) Obstructive sleep apnea is underrecognized and underdiagnosed in patients undergoing bariatric surgery. Eur Arch Oto-Rhino-Laryngol 269:1865–1871. https://doi.org/10.1007/s00405-012-1948-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Kyle D. Hunt, Aristithes G. Doumouras, Yung Lee, Scott Gmora, Mehran Anvari, and Dennis Hong have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hunt, K.D., Doumouras, A.G., Lee, Y. et al. The effect of surrogate procedure volume on bariatric surgery outcomes: do common laparoscopic general surgery procedures matter?. Surg Endosc 34, 1278–1284 (2020). https://doi.org/10.1007/s00464-019-06897-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06897-6