Abstract
Background
The influence of visual-spatial discordance during training on laparoscopic skills is poorly understood. It has been proposed that training in visual-spatial discordant situations can improve performance in the forward alignment, which was the basis of our hypothesis. Our study’s aim was to conduct a randomized control trial to explore the impact of simulated training in visual-spatial discordant situations on forward alignment performance.
Methods
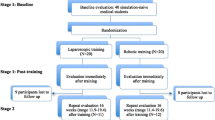
The participants were 80 medical students who were randomized into four groups. Group A served as the control and performed all peg transfers in the forward alignment. Groups B, C, and D experienced varied rounds of either increasing or decreasing sensorimotor discordance. The students were trained and tested using the peg transfer task used in the Fundamentals of Laparoscopic Surgery curriculum. Based on the group, each student performed 10 peg transfer practice rounds in their assigned alignment. After each practice session, each student was tested and scored in forward alignment performance. A baseline test, followed by three practice sessions, and three tests were done.
Results
Group A (control) demonstrated a statistically significant overall increase in scoring of 37.1% from baseline when compared to the final test. Groups B, C, and D showed improvements of 3.7%, 27.1%, and 19.3%, respectively, between baseline and the final test, yet none demonstrated consistent linear improvements. On multi-variate analysis, students who practiced in the side or reverse alignment positions scored 25 and 37 points lower, respectively, than students who practiced in the forward alignment.
Conclusion
Our study suggests that training in visual-spatial discordant conditions does not lead to the development of forward alignment laparoscopic skills. This could have important implications when developing future laparoscopic skills training curriculums. To our knowledge, this is the largest study to date assessing the impacts of training in visual-spatial discordance situations on performance in the forward alignment.

Similar content being viewed by others
References
Rhee R, Fernandez G, Bush R, Seymour NE (2014) The effects of viewing axis on laparoscopic performance: a comparison of non-expert and expert laparoscopic surgeons. Surg Endosc 28(9):2634–2640. https://doi.org/10.1007/s00464-014-3515-9
Conrad J, Shah AH, Divino CM, Schluender S, Gurland B, Shlasko E, Szold A (2006) The role of mental rotation and memory scanning on the performance of laparoscopic skills: a study on the effect of camera rotational angle. Surg Endosc 20(3):504–510. https://doi.org/10.1007/s00464-005-0363-7
Dunnican WJ, Singh TP, Ata A, Bendana EE, Conlee TD, Dolce CJ, Ramakrishnan R (2010) Reverse alignment “mirror image” visualization as a laparoscopic training tool improves task performance. Surg Innov 17(2):108–113. https://doi.org/10.1177/1553350610365346
Nagendran M, Toon CD, Davidson BR, Gurusamy KS (2014) Laparoscopic surgical box model training for surgical trainees with no prior laparoscopic experience. Cochrane Database Syst Rev (1):CD010479. https://doi.org/10.1002/14651858.cd010479.pub2
Zendejas B, Brydges R, Hamstra SJ, Cook DA (2013) State of the evidence on simulation-based training for laparoscopic surgery: a systematic review. Ann Surg 257(4):586–593. https://doi.org/10.1097/SLA.0b013e318288c40b
Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, Hoffman K, Committee SF (2004) Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 135(1):21–27. https://doi.org/10.1016/S0039
Holznecht C, Schmidt T, Gould J (2012) The impact of training under different visual-spatial conditions on reverse-alignment laparoscopic skills development. Surg Endosc 26(1):120–123. https://doi.org/10.1007/s00464-011-1836-5
Duarte RJ, Cury J, Oliveira LC, Srougi M (2013) Establishing the minimal number of virtual reality simulator training sessions necessary to develop basic laparoscopic skills competence: evaluation of the learning curve. Int Braz J Urol 39(5):712–719. https://doi.org/10.1590/S1677-5538.IBJU.2013.05.14
Peters M, Laeng B, Latham K, Jackson M, Zaiyouna R, Richardson C (1995) A redrawn Vandenberg and Kuse mental rotations test: different versions and factors that affect performance. Brain Cogn 28(1):39–58. https://doi.org/10.1006/brcg.1995.1032
Hwang MR, Seo GJ, Yoo SB, Park JW, Choi HS, Oh JH, Jeong SY (2010) Learning curve of assistants in laparoscopic colorectal surgery: overcoming mirror imaging. Surg Endosc 24(10):2575–2580. https://doi.org/10.1007/s00464-010-1005-2
Johnston WK 3rd, Low RK, Das S (2003) Image converter eliminates mirror imaging during laparoscopy. J Endourol 17(5):327–331. https://doi.org/10.1089/089277903322145521
Cresswell AB, Macmillan AI, Hanna GB, Cuschieri A (1999) Methods for improving performance under reverse alignment conditions during endoscopic surgery. Surg Endosc 13(6):591–594
Acknowledgements
This research project was supported in part by a grant from the Graduate Medical Education, Inc. (GMEI) Resident-led Research Mini-Grant Program, and an NIH (National Institutes of Health) grant award R25HL108864-01 to Elahé Crockett. Nashwa Khogali-Jakary was a 2013 NIH-National Heart, Lung and Blood Institute (NIH-NHLBI) scholar, and her research training was supported through the above NIH award (5-R25HL108864-01).
Funding
Funding received from the National Institutes of Health: National Heart, Lung and Blood Institute (NIH-NHLBI) award (Grant Number: 5-R25HL108864-01) to Elahé Crockett, Ph.D., MS, and Graduate Medical Education, Inc. (GMEI) Resident-led Research Mini-Grant Program (Grant Number: DS100069)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Nashwa Khogali-Jakary discloses that she reports grants from the National Heart, Lung, Blood Institute, during the conduct of the study. Drs. John Kanitra, Alan Davis, David Henry, Elahé T. Crockett, Srinivas Kavuturu, as well as Ms. Pamela Haan, Mr. Rama Gupta, Ms. Cheryl Anderson, Ms. Caroline Moon, and Ms. Terry McLeod have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khogali-Jakary, N., Kanitra, J.J., Haan, P.S. et al. Laparoscopic Simulation in Reverse and Side Alignment Impact on Forward Alignment Performance: A Randomized Controlled Trial. Surg Endosc 34, 298–303 (2020). https://doi.org/10.1007/s00464-019-06766-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06766-2