Abstract
Background
Single-incision laparoscopic surgery (SILS) is growing in popularity. The increased diameter of the umbilical incision might raise questions about the possibility of a greater risk of postoperative incisional hernia in comparison to conventional laparoscopy. This study aims to disclose the frequency of incisional hernia after SILS in long-term follow-up as well as to reveal the factors predisposing patients to this feared complication.
Methods
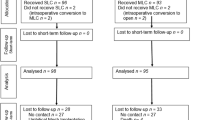
The patient collective consists of cholecystectomy and appendectomy patients, who were operated on using SILS technique. Follow-up was achieved through letter correspondence, telephone interview, and clinical examination. Effects of demographic variables and operative parameters including age, sex, BMI, ASA score, duration of surgery, pre-existing hernia as well as postoperative incidence of incisional hernia were investigated using univariate and multivariate analyses.
Results
A total of 286 cases with complete follow-up were included in the analyses. Mean follow-up duration was 58.4 months. 192 patients (67.1%) underwent cholecystectomy; 94 (32.9%) had an appendectomy. The study collective consisted of 218 women (76.2%) and 68 men (23.8%). Mean age at the date of the operation was 38.5 (median 36, range 13–74). In 5 cases (1.7%), the surgical approach was converted into conventional laparoscopy. Intraoperative complication rate was 0.3% and postoperative complication rate was 5.9%. 7 patients (2.4%) developed an incisional hernia. Obese patients had an incisional hernia incidence of 10.9%. 3 out of 19 patients (15.8%) with a pre-existing umbilical hernia developed an incisional hernia during follow-up. Obesity and pre-existing umbilical hernia proved to have a significant association with incisional hernia incidence in univariate and multivariate analyses. Sex, age, procedure (appendectomy vs cholecystectomy), presence of acute inflammation, and duration of surgery did not show a statistically significant association with incisional hernia.
Conclusion
Detection of incisional hernia necessitates a long follow-up duration. Obesity and pre-existing umbilical hernia are associated with a higher incidence of this complication. Following a careful patient selection, SILS offers a safe approach for cholecystectomy and appendectomy procedures.
Similar content being viewed by others
References
Julliard O, Hauters P, Possoz J, Malvaux P, Landenne J, Gherardi D (2016) Incisional hernia after single-incision laparoscopic cholecystectomy: incidence and predictive factors. Surg Endosc 30:4539–4543
Marks JM, Phillips MS, Tacchino R, Roberts K, Onders R, DeNoto G, Gecelter G, Rubach E, Rivas H, Islam A, Soper N, Paraskeva P, Rosemurgy A, Ross S, Shah S (2013) Single-incision laparoscopic cholecystectomy is associated with improved cosmesis scoring at the cost of significantly higher hernia rates: 1-year results of a prospective randomized, multicenter, single-blinded trial of traditional multiport laparoscopic cholecystectomy vs single-incision laparoscopic cholecystectomy. J Am Coll Surg 216:1037–1047 (discussion 1047–1038)
Bliss LA, Yang CJ, Kent TS, Ng SC, Critchlow JF, Tseng JF (2015) Appendicitis in the modern era: universal problem and variable treatment. Surg Endosc 29:1897–1902
Bunting DM (2010) Port-site hernia following laparoscopic cholecystectomy. J Soc Laparoendosc Surg 14:490–497
Buckley FP III, Vassaur HE, Jupiter DC, Crosby JH, Wheeless CJ, Vassaur JL (2016) Influencing factors for port-site hernias after single-incision laparoscopy. Hernia 20:729–733
Agaba EA, Rainville H, Ikedilo O, Vemulapali P (2014) Incidence of port-site incisional hernia after single-incision laparoscopic SURGERY. J Soc Laparoendosc Surg 18:204–210
Gunderson CC, Knight J, Ybanez-Morano J, Ritter C, Escobar PF, Ibeanu O, Grumbine FC, Bedaiwy MA, Hurd WW, Fader AN (2012) The risk of umbilical hernia and other complications with laparoendoscopic single-site surgery. J Minim Invasive Gynecol 19:40–45
Weiss HG, Brunner W, Biebl MO, Schirnhofer J, Pimpl K, Mittermair C, Obrist C, Brunner E, Hell T (2014) Wound complications in 1145 consecutive transumbilical single-incision laparoscopic procedures. Ann Surg 259:89–95
Krajinovic K, Koeberlein C, Germer CT, Reibetanz J (2016) The incidence of trocar site hernia after single-port laparoscopic cholecystectomy: a single center analysis and literature review. J Laparoendosc Adv Surg Techn A 26:536–539
Haueter R, Schutz T, Raptis DA, Clavien PA, Zuber M (2017) Meta-analysis of single-port versus conventional laparoscopic cholecystectomy comparing body image and cosmesis. Br J Surg 104:1141–1159
Swank HA, Mulder IM, la Chapelle CF, Reitsma JB, Lange JF, Bemelman WA (2012) Systematic review of trocar-site hernia. Br J Surg 99:315–323
Antoniou SA, Morales-Conde S, Antoniou GA, Granderath FA, Berrevoet F, Muysoms FE (2016) Single-incision laparoscopic surgery through the umbilicus is associated with a higher incidence of trocar-site hernia than conventional laparoscopy: a meta-analysis of randomized controlled trials. Hernia 20:1–10
Baucom RB, Ousley J, Feurer ID, Beveridge GB, Pierce RA, Holzman MD, Sharp KW, Poulose BK (2016) Patient reported outcomes after incisional hernia repair-establishing the ventral hernia recurrence inventory. Am J Surg 212:81–88
Nassar AH, Ashkar KA, Rashed AA, Abdulmoneum MG (1997) Laparoscopic cholecystectomy and the umbilicus. Br J Surg 84:630–633
Mayol J, Garcia-Aguilar J, Ortiz-Oshiro E, De-Diego Carmona JA, Fernandez-Represa JA (1997) Risks of the minimal access approach for laparoscopic surgery: multivariate analysis of morbidity related to umbilical trocar insertion. World J Surg 21:529–533
Comajuncosas J, Hermoso J, Gris P, Jimeno J, Orbeal R, Vallverdu H, Lopez Negre JL, Urgelles J, Estalella L, Pares D (2014) Risk factors for umbilical trocar site incisional hernia in laparoscopic cholecystectomy: a prospective 3-year follow-up study. Am J Surg 207:1–6
Gangl O, Hofer W, Tomaselli F, Sautner T, Fugger R (2011) Single incision laparoscopic cholecystectomy (SILC) versus laparoscopic cholecystectomy (LC): a matched pair analysis. Langenbecks Arch Surg 396:819–824
Christoffersen MW, Brandt E, Oehlenschlager J, Rosenberg J, Helgstrand F, Jorgensen LN, Bardram L, Bisgaard T (2015) No difference in incidence of port-site hernia and chronic pain after single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: a nationwide prospective, matched cohort study. Surg Endosc 29:3239–3245
Bury K, Pawlak M, Smietanski M, Muysoms F (2016) Single-incision port-site herniation: meta-analysis vs. nationwide cohort study. Hernia 20:11–12
Johnson WH, Fecher AM, McMahon RL, Grant JP, Pryor AD (2006) VersaStep trocar hernia rate in unclosed fascial defects in bariatric patients. Surg Endosc 20:1584–1586
Beck WC, Holzman MD, Sharp KW, Nealon WH, Dupont WD, Poulose BK (2013) Comparative effectiveness of dynamic abdominal sonography for hernia vs computed tomography in the diagnosis of incisional hernia. J Am Coll Surg 216:447–453 (quiz 510–441)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Mr. Barutcu and Klein, as well as Drs. Kilian, Biebl, Raakow, Pratschke, and Raakow have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barutcu, A.G., Klein, D., Kilian, M. et al. Long-term follow-up after single-incision laparoscopic surgery. Surg Endosc 34, 126–132 (2020). https://doi.org/10.1007/s00464-019-06739-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06739-5